DOI: 10.12809/hkmj144262
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Fatal bilateral lower-limb deep vein thrombosis and pulmonary embolism following single digit replantation
Anderson SM Leung, MB, BS, MHKICBSC;
Margaret WM Fok, FRCSEd(Orth), FHKAM (Orthopaedic Surgery);
Boris KK Fung, FRCSEd(Orth), FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and Traumatology, Queen Mary Hospital,
Pokfulam, Hong Kong
Corresponding author: Dr Margaret WM Fok (margaret_fok@yahoo.com)
Abstract
Venous thromboembolism in hand surgery is rare.
There is no report in the literature on postoperative
mortality from venous thromboembolism following
microsurgery in upper limbs. We report the case
of a 56-year-old Chinese man who died from
pulmonary embolism as a result of bilateral lower-limb
deep vein thrombosis following prolonged
surgery under general anaesthesia after replantation
of a finger. This case raises awareness of the need
for precautions against venous thromboembolism
following prolonged microsurgery and identification of high-risk patients.
Introduction
Venous thromboembolism (VTE) is a condition
that includes both deep vein thrombosis (DVT) and
pulmonary embolism (PE). The formation of thrombi
is associated with the Virchow’s triad, ie circulatory
stasis, vascular wall injury, and a hypercoagulable
state. Most data of VTE in orthopaedic surgeries
are based on studies of patients who undergo hip or
knee arthroplasty. The risk of VTE following lower-limb
surgery is noted to be considerably higher than
those following upper-limb surgery. To date, there
has been no evidence to support the prescription of
VTE prophylaxis in upper-limb operations.
Case report
In June 2013, a 56-year-old, non-obese, Chinese
carpenter, who enjoyed good past health and was a
non-smoker, sustained injuries to both his left ring
finger and little finger while using an electric saw.
His left ring finger was amputated at the level of
the middle phalanx and his little finger was nearly
amputated at the distal interphalangeal joint level.
No other site of injury was noted (Fig a). He presented
to our hospital 1 hour after the injury. Upon arrival
he was haemodynamically stable.
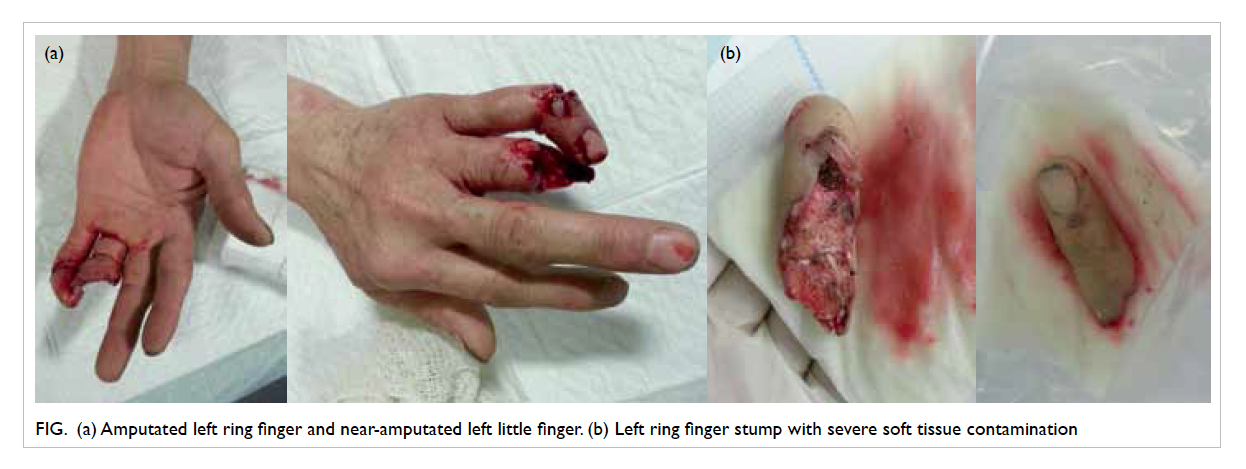
Figure. (a) Amputated left ring finger and near-amputated left little finger. (b) Left ring finger stump with severe soft tissue contamination
Due to the severe soft tissue contamination
of the finger stumps (Fig b), options of either replantation or revision amputation for the ring
finger was discussed with the patient. Subsequent
emergency operation was arranged for attempted
replantation of his ring finger, and wound
debridement and fixation of his left little finger.
Revascularisation of the ring finger was attempted
thrice, including use of a vein graft. However, due
to the inability to achieve sustained blood flow to
the amputated stump, revision amputation was
performed. Meanwhile, the open wound of the little
finger was debrided, and the fracture of the finger was
temporarily fixed with axial K wire. The operation
lasted 6 hours 25 minutes, with a total anaesthetic
time of 7 hours 12 minutes. The fluid balance was
+2450 mL. He regained full consciousness in the
recovery room, with good breathing and oxygen
saturation. Antibiotics were continued and he was
transferred back to a general ward.
The operation was completed at 4 am the next
day and his vital signs remained stable throughout.
He offered no complaints in the morning round
and was able to mobilise and walk to the washroom
where he sustained an unwitnessed fall. He had
neither preceding chest pain, headache, nor
swelling and pain over his lower limbs, and did
not lose consciousness. He developed tachycardia,
tachypnoea, and desaturation after being helped to
his bed. Echocardiogram revealed sinus tachycardia.
He started developing chest discomfort with
subsequent witnessed arrest 40 minutes later.
Cardiac monitoring revealed pulseless electrical
activity. Cardiopulmonary resuscitation was started
immediately with injection of adrenaline. Bedside
echocardiogram revealed no pericardial effusion
but there was no response to resuscitation and the
patient succumbed 35 minutes later. Postmortem
examination revealed bilateral DVT in the calf
muscles. Both lungs were markedly congested, with
occluding thromboemboli noted in the hilar main
pulmonary arteries and their main branches. No
other thromboemboli were noted.
Discussion
Lower limb surgery is a risk factor for VTE events.
The prevalence of DVT in patients who undergo hip
fracture surgery and hip or knee arthroplasty ranges
from 40% to 60%.1 2 Clinical or fatal PE in Hong Kong Chinese patients is even rarer.2
With regard to VTE following upper-limb
surgery, nine VTE events have been reported.
These comprised seven PEs following total elbow
arthroplasty (of which three were fatal), one non-fatal
PE after distal radius fixation following acute
fracture, and one non-fatal PE following revision
osteosynthesis of the proximal diaphysis of ulna.3
There has been no reported incidence in the
literature of VTE following microsurgery.
It is difficult to determine whether
microsurgery is completely risk-free for VTE.
Prolonged surgery may involve prolonged
immobilisation and blood loss that in turn increases
the risk of VTE, based on Virchow’s triad. It is thus
possible that prophylaxis for VTE is necessary in
microsurgery when the operating time is expected to
be long, for instance, in finger replantations or free-flap
surgeries.
Currently there is no guideline on VTE
prophylaxis for microsurgeries. The British Society
for Surgery of the Hand4 considers upper-limb
procedures under general anaesthesia for more than
90 minutes and/or with one risk factor for VTE (Box3)
as moderate-risk procedures. It recommends use of
mechanical compression devices in the operating
room and/or until the patient becomes ambulatory.
With the risk of bleeding in mind, low-molecular-weight
heparin (LMWH) may be started no less
than 6 hours postoperatively in selected patients and
continued until they are fully ambulatory.3 None of
these recommendations apply specifically to hand or
microsurgeries.
In addition to LMWH, the National Institute
for Health and Care Excellence clinical guideline
and the American College of Chest Physicians
(ACCP) also mention the newer non–vitamin K
antagonist oral anticoagulants (NOACs).5 This
group of drugs is associated with a rapid onset
of action and predictable pharmacokinetics and
pharmacodynamics. There are also fewer interactions
with food and other drugs. The ACCP recommends
the use of VTE prophylaxis for a minimum of 10
to 14 days following major orthopaedic surgery. In
patients who undergo total joint replacement, the
ACCP suggests the use of LMWH in preference
to other agents (eg fondaparinux, apixaban,
dabigatran, rivaroxaban, low-dose unfractionated
heparin, adjusted-dose vitamin K antagonist or
aspirin), irrespective of the concomitant use of an
intermittent pneumatic compression device. For
those patients who refuse injections, apixaban
or dabigatran is recommended. However, the
available studies (eg RE-MODEL trial, RECORD
trial and ADVANCE-2 study) and guidelines for
VTE prophylaxis focus on total joint replacement
surgeries.6 There are no recommendations on the
use of NOACs in microsurgeries.
When prescribing VTE prophylaxis, it is
important to balance the associated benefits and
risks. In the case of mechanical compression, in
view of its low-risk profile, it should be offered to
all patients who undergo prolonged microvascular
procedures, for example replantation, until they
are fully ambulatory. The application of mechanical
compression on both lower limbs may nonetheless
be limited if donor sites for blood vessels and other
tissues are anticipated from a lower limb.
Based on available evidence, we suggest that
all patients who undergo microsurgery should have
mechanical compression prophylaxis. Additional
pharmacological prophylaxis should be considered
for those who are at relatively high risk of developing
VTE, for example, patients who have more than
one risk factor, those in whom upper limb or tumour
surgery will exceed 90-minute duration, and/or
those in whom there will be prolonged postoperative
immobilisation.
References
1. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133(6 Suppl):381S-453S.
2. Mok CK, Hoaglund FT, Rogoff SM, Chow SP, Ma A, Yau AC. The incidence of deep vein thrombosis in Hong Kong Chinese after hip surgery for fracture of the proximal femur. Br J Surg 1979;66:640-2. Crossref
3. Roberts DC, Warwick DJ. Venous thromboembolism following elbow, wrist and hand surgery: a review of the literature and prophylaxis guidelines. J Hand Surg Eur Vol 2014;39:306-12. Crossref
4. The British Society for Surgery of the Hand. VTE Guidelines. Available from: http://www.bssh.ac.uk/education/guidelines/vteguidelines. Accessed 2 Jul 2012.
5. Beyer-Westendorf J, Ageno W. Benefit-risk profile of non–vitamin K antagonist oral anticoagulants in the management of venous thromboembolism. Thromb Haemost 2015;113:231-46. Crossref
6. Saraf K, Morris P, Garg P, Sheridan P, Storey R. Non–vitamin K antagonist oral anticoagulants (NOACs): clinical evidence and therapeutic considerations. Postgrad Med J 2014;90:520-8. Crossref