Hong Kong Med J 2015 Jun;21(3):243–50 | Epub 22 May 2015
DOI: 10.12809/hkmj144404
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Double balloon catheter for induction of labour in Chinese women with previous caesarean
section: one-year experience and literature review
Queenie KY Cheuk, MB, ChB, FHKAM (Obstetrics and Gynaecology)1;
TK Lo, MB, BS, FHKAM (Obstetrics and Gynaecology)2;
CP Lee, FRCOG, FHKAM (Obstetrics and Gynaecology)2;
Anita PC Yeung, FRCOG, FHKAM (Obstetrics and Gynaecology)1
1 Department of Obstetrics and Gynaecology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
2 Department of Obstetrics and Gynaecology, Queen Mary Hospital, The University of Hong Kong, Pokfulam, Hong Kong
Corresponding author: Dr Queenie KY Cheuk (cheuky3@ha.org.hk)
Abstract
Objectives: To evaluate the efficacy and safety of
double balloon catheter for induction of labour in
Chinese women with one previous caesarean section
and unfavourable cervix at term.
Design: Retrospective cohort study.
Setting: A regional hospital in Hong Kong.
Patients: Women with previous caesarean
delivery requiring induction of labour at term and with an unfavourable cervix from May 2013 to April
2014.
Major outcome measures: Primary outcome
was to assess rate of successful vaginal delivery
(spontaneous or instrument-assisted) using double
balloon catheter. Secondary outcomes were double
balloon catheter induction-to-delivery and removal-to-delivery interval; cervical score improvement;
oxytocin augmentation; maternal or fetal
complications during cervical ripening, intrapartum
and postpartum period; and risk factors associated
with unsuccessful induction.
Results: All 24 Chinese women tolerated double
balloon catheter well. After double balloon catheter
expulsion or removal, the cervix successfully ripened
in 18 (75%) cases. The improvement in Bishop
score 3 (interquartile range, 2-4) was statistically
significant (P<0.001). Overall, 18 (75%) cases were
delivered vaginally. The median insertion-to-delivery
and removal-to-delivery intervals were
19 (interquartile range, 13.4-23.0) hours and 6.9 (interquartile range, 4.1-10.8) hours, respectively.
Compared with cases without, the interval to delivery
was statistically significantly shorter in those with
spontaneous balloon expulsion or spontaneous
membrane rupture during ripening (7.8 vs 3.0
hours; P=0.025). There were no major maternal or
neonatal complications. The only factor significantly
associated with failed vaginal birth after caesarean
was previous caesarean section for failure to progress
(P<0.001).
Conclusions: This is the first study using double
balloon catheter for induction of labour in Asian
Chinese women with previous caesarean section.
Using double balloon catheter, we achieved a vaginal
birth after caesarean rate of 75% without major
complications.
New knowledge added by this
study
- This is the first report from Asian Chinese women on the use of double balloon catheter (DBC) for induction of labour in the presence of a caesarean scar. Using DBC, a vaginal birth after caesarean (VBAC) rate of 75% was achieved without major complications.
- During cervical ripening with DBC, cases with spontaneous balloon expulsion or spontaneous membrane rupture had a more favourable outcome with shorter interval to delivery.
- Previous caesarean section for failure to progress was significantly associated with failed VBAC.
- Our anecdotal experience with DBC was favourable and its application may reduce repeated caesarean section rates. Further research exploring this potential is warranted and large randomised controlled trials are needed to confirm its efficacy.
Introduction
There is widespread public and professional concern
about the increasing rates of caesarean section (CS).
In the UK and North America, around 25% and 32%
of births respectively were by CS.1 2 In Hong Kong,
according to the 2009 territory-wide O&G audit
report, CS rate has been around 42.1%.3 Previous CS
has been the most common indication for caesarean
delivery.3 In subsequent pregnancies, CS can be
associated with serious maternal morbidities.4 To
reduce CS rate and related morbidities, vaginal birth
after caesarean (VBAC) is an alternative advocated
in most developed countries.2 5 6 According to the
UK and North American guidelines, induction of
labour (IOL) can be offered to women with medical
or obstetric indications who opt for VBAC after
discussion.2 5
Unfavourable cervix, which is a common
obstetric problem, can be addressed using
pharmacological and mechanical methods to enable
cervical ripening. In Hong Kong pharmacological
method is more commonly used for IOL. In
women with previous CS, the increased risk of
uterine rupture is a major concern during IOL.2 5 6 7
Mechanical methods apply pressure on the internal
cervical os, stretch the lower uterine segment, and
increase local production of prostaglandin. There is
a lack of compelling evidence suggesting increased
risk of uterine rupture because mechanical devices
can be readily removed when needed and are stable
in room temperature. Compared to conventional
Foley catheter, the double balloon catheter (DBC)
has a cervicovaginal balloon in addition, allowing
greater compression of the cervical os and avoiding
the need for traction (Fig 1). Nevertheless, there are limited reports about the experience with the use of
DBC. Regarding the question of which IOL method is
suitable in women with prior CS, a recent Cochrane
review stated that there was insufficient information
available to conclude on the optimal method of IOL
in women with prior CS.7
Since May 2013, our unit has been offering
the option of DBC (Cook Cervical Ripening
Balloon; Cook Medical, Bloomington [IN], US) for
IOL in women with one previous CS. Therefore,
we conducted a study on Chinese women with an
objective to evaluate the efficacy and safety of the
DBC in IOL with one previous CS and unfavourable
cervix at term. Another objective was to identify
risk factors associated with unsuccessful VBAC. This
is one of the first studies to report using DBC for this
indication in Asian Chinese population.
Methods
This retrospective study was conducted in the
obstetrics unit of Pamela Youde Nethersole Eastern
Hospital in Hong Kong. The unit provides tertiary
care and conducts over 3000 deliveries per year. Prior
to the introduction of DBC, the background CS and
VBAC rates in our unit was approximately 30% and
1.9%, respectively. The overall success rate of VBAC
was more than 80%. In our study, we identified VBAC
cases using DBC for IOL between 1 May 2013 and
30 April 2014 through the departmental database.
Clinical details were reviewed from the case notes
and hospital electronic systems.
Inclusion and exclusion criteria
Inclusion criteria were women with one lower
transverse caesarean scar and no contra-indication
for VBAC who were given the option of either
repeated elective CS or VBAC. Those VBAC cases
requiring medically or obstetrically indicated IOL
were offered DBC if the cervix was unfavourable
(modified Bishop score <6) and membranes intact.
The exclusion criteria for using DBC were:
women with two or more previous CS, classical
CS scar, inverted T or J or low vertical incision in
previous CS; previous uterine scar for gynaecological
conditions, eg myomectomy, hysterotomy;
congenital uterine abnormality; twin pregnancy,
non-cephalic presentations, intra-uterine death,
suspected fetal distress; uterine fibroids which
may obstruct labour, placenta praevia, antepartum
haemorrhage, leaking, clinical chorioamnionitis,
suspected macrosomia (ultrasound estimated fetal
weight ≥4000 g), polyhydramnios (amniotic fluid
index ≥25 cm or single deepest pocket ≥8 cm),
congenital fetal abnormalities; and maternal diseases
or maternal infection which would contra-indicate
vaginal delivery or warrant prompt delivery. Ethical
approval for this study was obtained from the local
institutional human research ethics committee.
Induction-of-labour protocol
Eligible patients were admitted into hospital in the
evening and an initial Bishop score was obtained.
Cardiotocogram for 60 minutes, and ultrasound scan
to assess estimated fetal weight, liquor volume, fetal
wellbeing by umbilical artery Doppler and placental
location were performed. After informed consent, the
DBC was inserted according to the manufacturer’s
instruction. If the DBC insertion failed, women
would be offered CS the next day morning. The
procedure of DBC insertion in all patients was done
by one investigator (KY Cheuk). The uterine and
vaginal balloons were inflated in phases to 40-50
mL and 60 mL, respectively using normal saline.
After insertion, vaginal examination was performed
to confirm correct placement. The catheter was
taped to the woman’s inner thigh without tension.
Following insertion of catheter, continuous fetal
heart monitoring (CFHM) was done for 60 minutes.
The catheter was kept for 12 hours if spontaneous
expulsion did not occur, or removed earlier if there
was spontaneous rupture of membranes, excessive
vaginal bleeding, fetal distress, scar tenderness,
or patient intolerance. Immediately following
balloon expulsion or removal, the Bishop score was
reassessed, followed by an attempt to have artificial rupture of membranes (ARM) regardless of Bishop
score. To reduce the potential inter-observer bias,
the same investigator (KY Cheuk) assessed the
Bishop score before DBC insertion and immediately
after DBC expulsion or removal. Oxytocin infusion
(Syntocinon; Sandoz Pharmaceuticals, East Hanover
[NJ], US) was commenced if after ARM the uterine
contractions remained suboptimal at a rate of
1 mU/min and the infusion rate was doubled every
30 minutes until the uterine contractions were
regular at 3 minutes’ interval. The maximum dose
was capped at 8 mU/min. Oxytocin was not started
without membrane rupture or if the DBC was still
in place; CFHM was started after ARM till delivery.
Labour was managed by the attending obstetrician
and midwives. Assessment of labour progress and
administration of analgesia was made according to
departmental protocols. Group B streptococcus
prophylaxis was given according to departmental
protocol. It was commenced after DBC insertion
until delivery for group B streptococcus carriers.
Outcome measures
The primary outcome was successful vaginal
delivery (spontaneous or instrument-assisted). The
secondary outcomes were: induction-to-delivery
interval; device-removal-to-delivery interval;
cervical score improvement; oxytocin augmentation;
maternal or fetal complications during cervical
ripening, intrapartum and postpartum period, which
included failed device insertion, inability to void
during insertion, intolerance of device necessitating
early removal, uterine hyperstimulation, uterine
rupture, fetal distress, abruption, antepartum
haemorrhage, cord prolapse, malpresentation,
meconium-stained liquor, intrapartum and
postpartum infection, postpartum haemorrhage,
readmission in puerperium period, neonate delivery
with Apgar score of <7 in 5 minutes, cord blood pH
of <7.2, admission to neonatal intensive care unit,
neonatal sepsis, respiratory distress syndrome and
neonatal death, and risk factors associated with
unsuccessful induction.
Uterine hyperstimulation was defined as either
the occurrence of five or more contractions in 10
minutes for two consecutive 10-minute period, or
a contraction lasting for at least 2 minutes, with or
without changes in fetal heart rate pattern. Uterine
rupture was defined as disruption of the uterine
muscle extending to and involving the uterine serosa
or disruption of the uterine muscle with extension to
the bladder or broad ligament.5 Uterine dehiscence
was defined as disruption of the uterine muscle with
intact uterine serosa.5 Intrapartum infection was
defined by maternal fever of ≥38°C during labour.
Failed IOL was defined as failed ARM after catheter
removal or cervical dilatation of <3 cm after at least
8 hours of optimal uterine contractions.
Literature review
We also conducted a literature search on PubMed,
Ovid Medline, EMBASE, Cochrane library database
of systematic reviews and open library using the
keywords “double balloon catheter”, “Atad balloon”,
“double balloon device”, “Foley catheter”, “induction”,
“previous caesarean section”, and “previous scarred
uterus”. Bibliographies of all relevant articles
identified were searched manually to locate
additional studies. We excluded non-English
publications, or if the original paper was not available
from various sources such as PubMed, local hospital
or universities library systems and internet.
Statistical analyses
The statistical analysis was done by PASW Statistics
18, Release Version 18.0.0 (SPSS Inc, 2009, Chicago
[IL], US). Fisher’s exact test was used for categorical
data, while independent t test was used if normally
distributed, and non-parametric test (ie Mann-Whitney U test) if highly skewed. Univariate analysis
was used to assess the risk factors associated with
unsuccessful VBAC. To identify the differential
effect over time, Wilcoxon signed rank test was used
to compare the cervical Bishop scores before and
after DBC application. The critical level of statistical
significance was set at P<0.05.
Results
Twenty-five cases were identified during the 1-year
study period, and one non-Chinese woman’s data
were excluded. The remaining 24 cases were included
for analysis. Table 1 summarises the baseline
characteristics of study patients.
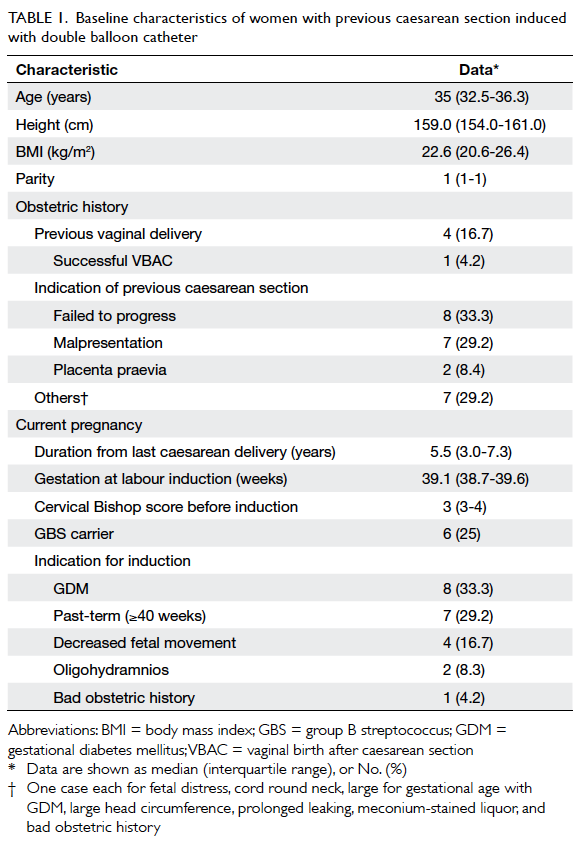
Table 1. Baseline characteristics of women with previous caesarean section induced with double balloon catheter
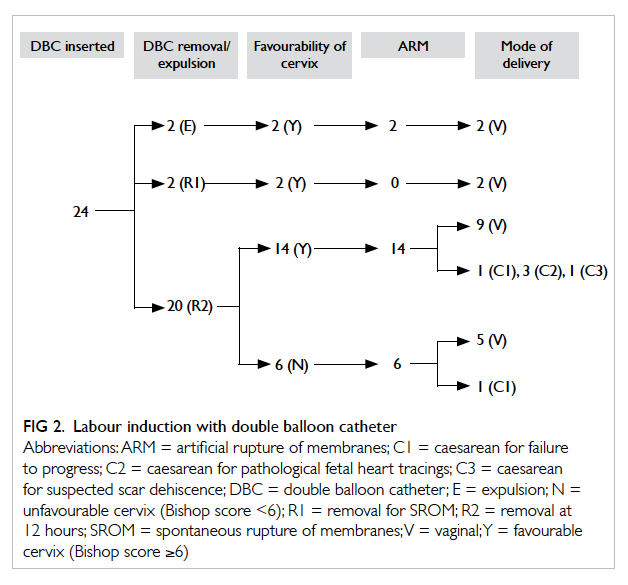
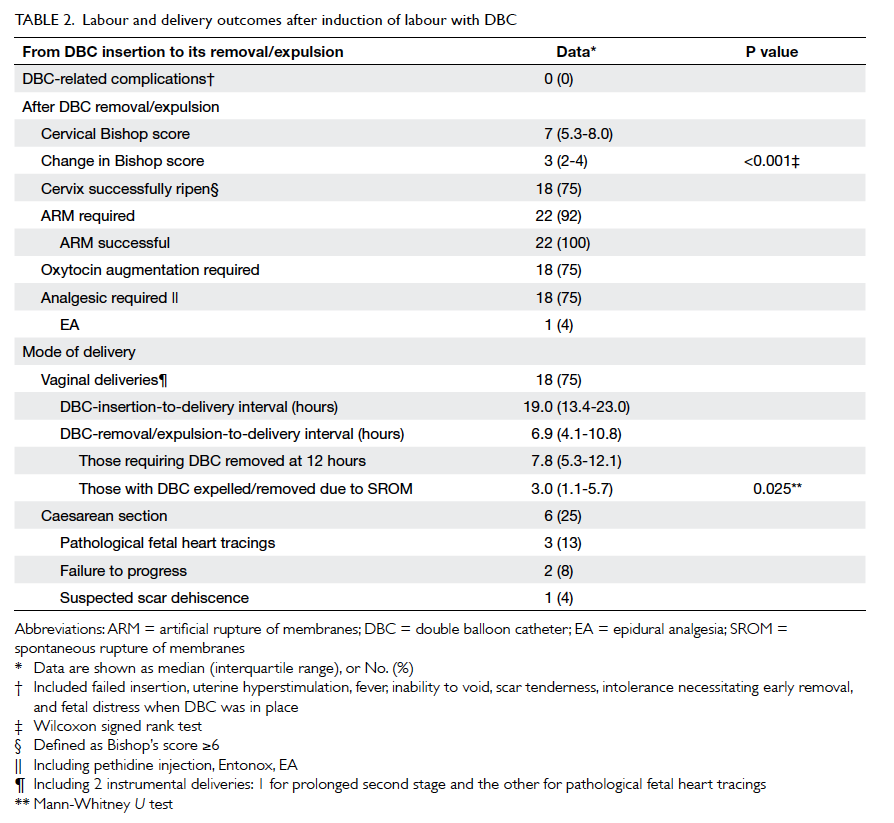
Figure 2 depicts the induction process and outcomes of the 24 cases; DBC was well tolerated
in all cases (Table 2). There was no case of failed insertion. After DBC expulsion or removal, the
cervix became favourable (Bishop’s score ≥6) in
18 (75%) cases. The improvement in Bishop score
3 (interquartile range [IQR], 2-4) was statistically
significant (P<0.001). Artificial rupture of the
membranes was successful in all 22 cases with intact
membranes, regardless of cervical favourability.
Oxytocin augmentation was required in 18 (75%)
cases. Overall, 75% of cases were delivered vaginally.
Among them, the median insertion-to-delivery
and removal-to-delivery intervals were 19 (IQR,
13.4-23.0) hours and 6.9 (IQR, 4.1-10.8) hours,
respectively. All the four women with previous
vaginal deliveries had successful VBAC. Compared
with cases without, the balloon expulsion-to-delivery
or removal-to-delivery interval was shorter in those
with spontaneous balloon expulsion or early balloon
removal due to spontaneous membrane rupture
during ripening (7.8 vs 3.0 hours, P=0.025). All the
cases had good neonatal outcomes with cord blood
pH of >7.25, 5-minute Apgar score of 10, without
the need for neonatal intensive care unit admissions
(Table 3). One case reported severe scar pain
during oxytocin augmentation. Scar dehiscence was
suspected and emergency CS performed. Dehiscence
was not substantiated intra-operatively. The baby
was born in good condition. Apart from a few cases
of maternal complications (eg postpartum infection
and postpartum haemorrhage), there was no case of
uterine rupture or adverse neonatal complications.
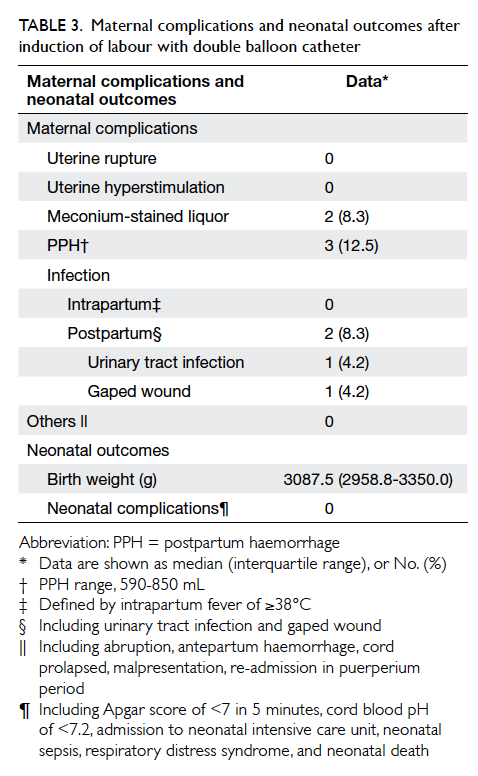
Table 3. Maternal complications and neonatal outcomes after induction of labour with double balloon catheter
To study the risk factors associated with
unsuccessful VBAC, univariate analysis was
performed using maternal age, height, body mass
index, cervical Bishop score, cervical favourability
after DBC removal or dislodgement, gender and
birth weight of baby, gestational diabetes mellitus,
history of vaginal delivery, history of successful
VBAC, inter-pregnancy interval, the indication
for previous CS, and the indication for IOL in the
current pregnancy as variables. Previous CS for
failure to progress was the only factor significantly
associated with unsuccessful VBAC (P<0.001).
Discussion
Few studies have investigated the use of DBC for
IOL in patients with previous caesarean scars.
Table 4 summarises the findings from some of the studies8 9 10 11 including the current study. Most of the
studies showed significant improvement in Bishop
score after using the device and a favourable cervix
was achieved in 75% to 85% of cases. The overall
vaginal delivery rate was 60.2% (71/118). There was
one (0.85%) case of symptomatic scar dehiscence,
and no adverse neonatal complications. The cervical
ripening success rate in our study was comparable to
those in other studies, and also our study achieved
a higher vaginal delivery rate. One explanation for
this would have been due to differences in the IOL
protocols. Some authors would offer CS directly
if the cervix failed to ripen after the DBC.9 Our
practice was to continue induction with ARM and
oxytocin even if the cervix remained unfavourable
after the DBC. In our patients, 83.3% (5/6) in this
group delivered vaginally with continued induction.
A second potential reason for better outcomes in our
study would lie in the differences in inclusion criteria.
Some studies had excluded women with previous
vaginal delivery,10 a factor known to be associated
with successful VBAC. A third reason could have
been differences in ethnicity. Studies have shown
that ethnicity does impact VBAC success rates.12
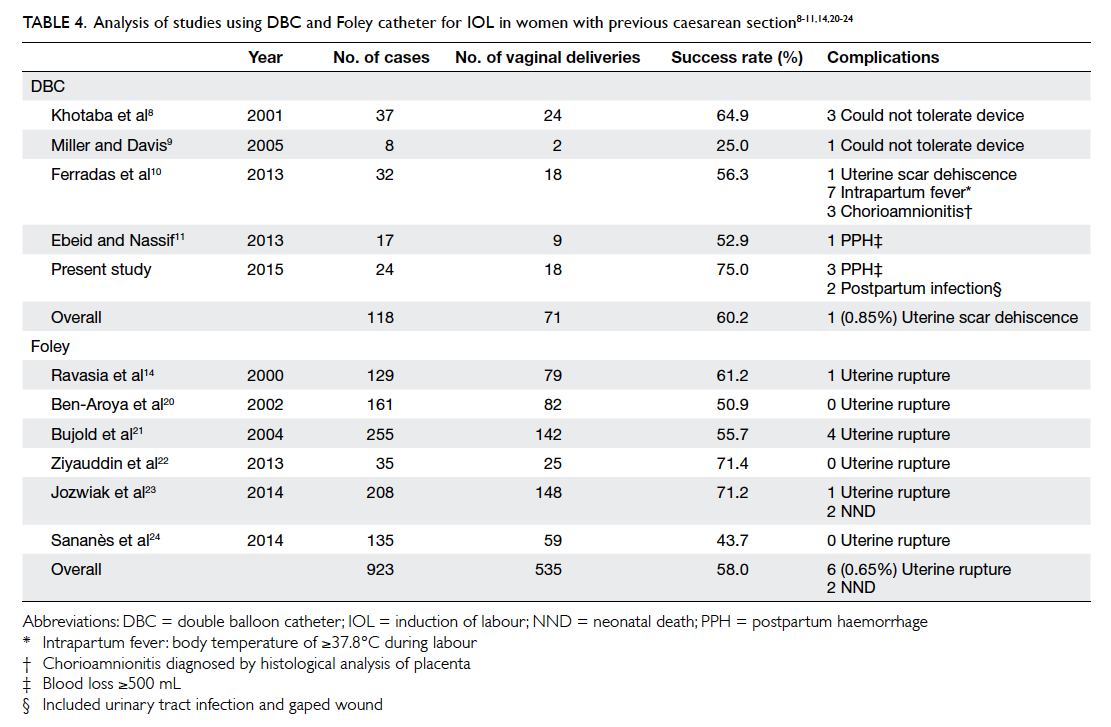
Table 4. Analysis of studies using DBC and Foley catheter for IOL in women with previous caesarean section8 9 11 14 20 21 22 23 24
With increasing rates of CS worldwide, it is
estimated that 10% of women requiring IOL have
a history of CS. However, the optimal induction
method for this high-risk group is unknown. To
counter unfavourable cervix with intact membranes,
prostaglandins and mechanical methods such
as Foley or DBC have been used. Prostaglandins
appeared to be associated with a higher uterine
rupture risk.13 14 Ravasia et al14 found that the relative
risk of uterine rupture with prostaglandins versus
spontaneous labour was 6.41, whereas the risk
with the use of Foley catheter was comparable to
spontaneous labour. Although infective morbidity
associated with mechanical induction is a concern,
the evidence is contradictory.15 16 A systematic
review by Heinemann et al15 on studies using Foley
catheter for IOL showed that use of mechanical
devices was associated with significant increase
in maternal morbidity due to infectious morbidity
when compared with pharmacological agents. On
the other hand, a recent Cochrane review showed no
increase in serious maternal morbidity with the use
of the Foley catheter.7 Further support was provided
from the recent open-label randomised controlled
trial PROBAAT,16 which compared Foley catheter
to vaginal prostaglandin in 824 women without
previous CS. The study showed that Foley catheter
had similar CS rates, less uterine hyperstimulation,
fewer maternal and fetal morbidities, and no increase
in infectious morbidity. Although Foley catheter
was featured in all these studies, DBC potentially
has additional utility for an unripe cervix as it
applies pressure on both the external and internal
os, avoiding the need for traction and reduces the
associated patient discomfort. Double balloon
catheter has a larger inflated volume compared
with Foley catheter (80 mL vs 30 mL) and therefore
IOL with a bigger balloon volume may shorten
duration of labour with better cervical dilatation.17
Nevertheless, clinical data comparing DBC with
Foley catheter in the presence of a caesarean scar are
lacking, while those on intact uterus are scarce and
inconclusive.18 19
Table 4 summarises the results of studies using Foley catheter for IOL in the presence of a caesarean
scar.14 20 21 22 23 24 It appears that DBC achieved comparable
vaginal delivery rate (60.2% vs 58.0%) and similar
uterine rupture/dehiscence rate (0.85 % vs 0.65%).
There was no case report of neonatal death in studies
using DBC while there were two cases reported with
Foley catheter. One was due to uterine rupture;
another was due to rupture of vasa praevia which was
independent of the method of induction.23 Further
research to compare the efficiency and safety of the
two devices for IOL in women with previous CS is
warranted. Although uterine rupture and infectious
morbidity seemed rare with DBC in women with
previous CS, the number of women studied was too
small to allow solid conclusion on its safety.
The complication rate for VBAC attempt was
highest in those who failed to achieve VBAC in the
end.25 Knowledge of the factors associated with
successful VBAC would therefore enable better
counselling on the choice of mode of delivery. Landon
et al12 in a large cohort of 14 529 women showed that
previous vaginal delivery and previous successful
VBAC were the best predictors of successful VBAC;
the success rates were 86.6% and 89.6%, respectively.
In our study, all four cases with previous vaginal
delivery (including one with previous VBAC) had
successful VBAC. In the study by Landon et al,12
factors associated with unsuccessful VBAC included
obesity, previous CS for dystocia, IOL, birth weight of
<4000 g, advanced maternal age, short stature, more
than 2 years from previous caesarean, gestational age
of ≥41 weeks, and previous preterm CS. Despite our
small sample size, we concurred that previous CS for
failure to progress was a significant factor associated
with unsuccessful VBAC.
Conclusions
This is the first report from East Asia on the use
of DBC for IOL in the presence of caesarean scar.
A success rate of 75% was achieved using VBAC
in Chinese women with a caesarean scar and an
unfavourable cervix. The procedure of DBC was
well tolerated, and no major complications were
observed. Our favourable experience with DBC
in Asian Chinese women lends support to further
research exploring the potential of this promising
modality in averting the rising CS rates in this part
of the world.
References
1. Caesarean section. NICE Clinical Guidelines. National
Collaborating Centre for Women’s and Children’s Health
(UK). London: RCOG Press; November 2011.
2. Vaginal birth after previous Caesarean delivery.
ACOG Practice Bulletin. No. 115. American College of
Obstetricians and Gynecologists; August 2010.
3. HKCOG Territory-wide O&G Audit Report: Caesarean
section. Hong Kong: Hong Kong College of Obstetricians
and Gynaecologists; 2009.
4. Bates GW Jr, Shomento S. Adhesion prevention in patients
with multiple cesarean deliveries. Am J Obstet Gynecol
2011;205(6 Suppl):S19-24. Crossref
5. Birth after previous Caesarean birth. RCOG Green-top
Guideline No. 45. Royal College of Obstetricians and
Gynaecologists; February 2007.
6. Society of Obstetricians and Gynaecologists of Canada.
SOGC clinical practice guidelines. Guidelines for vaginal
birth after previous caesarean birth. Number 155 (Replaces
guideline Number 147), February 2005. Int J Gynaecol
Obstet 2005;89:319-31.
7. Jozwiak M, Dodd JM. Methods of term labour induction
for women with a previous caesarean section. Cochrane
Database Syst Rev 2013;(3):CD009792. Crossref
8. Khotaba S, Volfson M, Tarazova L, et al. Induction of labor
in women with previous cesarean section using the double
balloon device. Acta Obstet Gynecol Scand 2001;80:1041-2. Crossref
9. Miller TD, Davis G. Use of the Atad catheter for the
induction of labour in women who have had a previous
Caesarean section—a case series. Aust N Z J Obstet
Gynaecol 2005;45:325-7. Crossref
10. Ferradas E, Alvarado I, Gabilondo M, Diez-Itza I, García-Adanez J. Double balloon device compared to oxytocin for
induction of labour after previous caesarean section. Open
J Obstet Gynecol 2013;3:212-6. Crossref
11. Ebeid E, Nassif N. Induction of labor using double balloon
cervical device in women with previous cesarean section:
experience and review. Open J Obstet Gynecol 2013;3:301-5. Crossref
12. Landon MB, Leindecker S, Spong CY, et al. The MFMU
Cesarean Registry: factors affecting the success of trial
of labor after previous cesarean delivery. Am J Obstet
Gynecol 2005;193:1016-23. Crossref
13. Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP.
Risk of uterine rupture during labor among women with a
prior cesarean delivery. N Engl J Med 2001;345:3-8. Crossref
14. Ravasia DJ, Wood SL, Pollard JK. Uterine rupture during
induced trial of labor among women with previous
cesarean delivery. Am J Obstet Gynecol 2000;183:1176-9. Crossref
15. Heinemann J, Gillen G, Sanchez-Ramos L, Kaunitz AM.
Do mechanical methods of cervical ripening increase
infectious morbidity? A systematic review. Am J Obstet
Gynecol 2008;199:177-87. Crossref
16. Jozwiak M, Oude Rengerink K, Benthem M, et al. Foley
catheter versus vaginal prostaglandin E2 gel for induction
of labour at term (PROBAAT trial): an open-label,
randomized controlled trial. Lancet 2011;378:2095-103. Crossref
17. Levy R, Kanengiser B, Furman B, Ben Arie A, Brown D,
Hagay ZJ. A randomized trial comparing a 30-mL and an
80-mL Foley catheter balloon for preinduction cervical
ripening. Am J Obstet Gynecol 2004;191:1632-6. Crossref
18. Salim R, Zafran N, Nachum Z, Garmi G, Kraiem N, Shalev
E. Single-balloon compared with double-balloon catheters
for induction of labor: a randomized controlled trial.
Obstet Gynecol 2011;118:79-86. Crossref
19. Mei-Dan E, Walfisch A, Valencia C, Hallak M. Making
cervical ripening EASI: a prospective controlled
comparison of single versus double balloon catheters. J
Matern Fetal Neonatal Med 2014;27:1765-70. Crossref
20. Ben-Aroya Z, Hallak M, Segal D, Friger M, Katz M, Mazor
M. Ripening of the uterine cervix in a post-cesarean
parturient: prostaglandin E2 versus Foley catheter. J
Matern Fetal Neonatal Med 2002;12:42-5. Crossref
21. Bujold E, Blackwell SC, Gauthier RJ. Cervical ripening with
transcervical foley catheter and the risk of uterine rupture.
Obstet Gynecol 2004;103:18-23. Crossref
22. Ziyauddin F, Hakim S, Beriwal S. The transcervical foley
catheter versus the vaginal prostaglandin e2 gel in the
induction of labour in a previous one caesarean section—a
clinical study. J Clin Diagn Res 2013;7:140-3. Crossref
23. Jozwiak M, van de Lest HA, Burger NB, Dijksterhuis MG,
De Leeuw JW. Cervical ripening with Foley catheter for
induction of labor after cesarean section: a cohort study.
Acta Obstet Gynecol Scand 2014;93:296-301. Crossref
24. Sananès N, Rodriguez M, Stora C, et al. Efficacy and safety
of labour induction in patients with a single previous
Caesarean section: a proposal for a clinical protocol. Arch
Gynecol Obstet 2014;290:669-76. Crossref
25. Landon MB, Hauth JC, Leveno KJ, et al. Maternal and
perinatal outcomes associated with a trial of labor after
prior cesarean delivery. N Engl J Med 2004;351:2581-9. Crossref