Hong Kong Med J 2015 Apr;21(2):98–106 | Epub 10 Mar 2015
DOI: 10.12809/hkmj144311
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Prospective study on the effects of orthotic treatment for medial knee osteoarthritis in Chinese patients: clinical outcome and
gait analysis
Henry CH Fu, MB, BS, MMedSc1;
Chester WH Lie, FRCS (Edin), FHKAM (Orthopaedic Surgery)2;
TP Ng, FRCS (Edin), FHKAM (Orthopaedic Surgery)3;
KW Chen, BSc4;
CY Tse, BSc4;
WH Wong, Diploma in Prosthetics and Orthotics4
1 Department of Orthopaedics and Traumatology, Queen Mary Hospital, Pokfulam, Hong Kong
2 Department of Orthopaedics and Traumatology, Kwong Wah Hospital, Yaumatei, Hong Kong
3 Private Practice, Hong Kong
4 Department of Prosthetics and Orthotics, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr Chester WH Lie (chesterliewh@gmail.com)
Abstract
Objective: To evaluate the effectiveness of various
orthotic treatments for patients with isolated medial
compartment osteoarthritis.
Design: Prospective cohort study with sequential
interventions.
Setting: University-affiliated hospital, Hong Kong.
Patients: From December 2010 to November
2011, 10 patients with medial knee osteoarthritis
were referred by orthopaedic surgeons for orthotic
treatment. All patients were sequentially treated
with flat insole, lateral-wedged insole, lateral-wedged
insole with subtalar strap, lateral-wedged
insole with arch support, valgus knee brace, and
valgus knee brace with lateral-wedged insole with
arch support for 4 weeks with no treatment break.
Three-dimensional gait analysis and questionnaires
were completed after each orthotic treatment.
Main outcome measures: The Western Ontario and
McMaster Universities Arthritis Index (WOMAC),
visual analogue scale scores, and peak and mean
knee adduction moments.
Results: Compared with pretreatment, the
lateral-wedged insole, lateral-wedged insole
with arch support, and valgus knee brace groups
demonstrated significant reductions in WOMAC
pain score (19.1%, P=0.04; 18.2%, P=0.04; and
20.4%, P=0.02, respectively). The lateral-wedged
insole with arch support group showed the greatest
reduction in visual analogue scale score compared
with pretreatment at 24.1% (P=0.004). Addition of
a subtalar strap to lateral-wedged insoles (lateral-wedged insole with subtalar strap) did not produce
significant benefit when compared with the lateral-wedged
insole alone. The valgus knee brace with
lateral-wedged insole with arch support group
demonstrated an additive effect with a statistically
significant reduction in WOMAC total score (-26.7%, P=0.01). Compliance with
treatment for the isolated insole groups were all
over 90%, but compliance for the valgus knee brace–associated groups was only around 50%. Gait analysis
indicated statistically significant reductions in peak
and mean knee adduction moments in all orthotic
groups when compared with a flat insole.
Conclusions: These results support the use of
orthotic treatment for early medial compartment
knee osteoarthritis.
New knowledge added by this
study
- Our data support the use of the lateral-wedged insole with arch support and valgus knee brace in the management of medial compartment osteoarthritis of the knee; however, compliance with the valgus knee brace is fair. Gait analysis showed that both supports can reduce the knee adduction moment during walking.
- Lateral-wedged insoles with arch support and valgus knee brace can be considered for patients with medial compartment osteoarthritis of the knee.
Introduction
Osteoarthritis of the knee is the commonest type
of arthritis affecting the geriatric population. Conservative treatment with physiotherapy and
analgesics provides temporary relief of symptoms,
yet surgical intervention such as high tibial
osteotomy, unicompartmental knee replacement, or
total knee replacement is a major undertaking and
not without risk.1 2 The medial compartment is more
commonly affected than the lateral compartment
in osteoarthritis (67% and 17%, respectively).3
Varus alignment of the lower limbs increases
the risk of incident knee osteoarthritis and also
increases the risk of disease progression in patients
with osteoarthritis.4 Apart from static lower limb
alignment, dynamic varus thrust during the gait cycle
is also independently associated with osteoarthritis
progression in the knee.5 Knee adduction moment
(KAM) is an indirect means to assess varus thrust
during the gait cycle. Previous studies have proven
the validity of KAM for prediction of clinical and
radiological osteoarthritis progression.6
Orthotic treatment can alter loading to
the knee in the hope of reducing symptoms and
disease progression. Biomechanical studies have
demonstrated a small effect size in reduction of
KAM with a valgus knee brace7 8 9 10 and lateral-wedged
insoles.11 12 13 14 This study is the first to sequentially
evaluate the clinical outcomes and gait analyses of
different orthotic treatments in Chinese patients
with medial compartment osteoarthritis.
Methods
Patients
From December 2010 to November 2011, 18
patients with isolated medial osteoarthritis of the
knee were referred by orthopaedic surgeons to the
Department of Prosthetics and Orthotics at Queen
Mary Hospital for orthotic treatment.
The inclusion criteria were age older than 50
years and a diagnosis of osteoarthritis according to
the American College of Rheumatology criteria.15
The predominant symptom needed to be medial
knee pain. Radiographical features needed to
include varus knee alignment and osteoarthritis of
Kellgren-Lawrence grade 2 or above over the medial
compartment.16
Our study population comprised patients with
isolated medial compartment osteoarthritis, while
patients with predominant lateral compartment
or patellofemoral joint symptoms or those with
radiographical features of osteoarthritis of
Kellgren-Lawrence grade 2 or above over the lateral
compartment or patellofemoral joint were excluded.
Patients with previous knee surgery, fixed
flexion deformity of >10°, hip or ankle pathology,
required a walking aid, or had morbid obesity (body
mass index, >40 kg/m2), a dermatological condition,
or peripheral vascular disease were also excluded.
This was a non-randomised prospective cohort
study with a cross-over design. All 10 patients were
sequentially treated with a flat insole (FI), lateral-wedged
insole (LW), lateral-wedged insole with
subtalar strap (LW+SS), lateral-wedged insole with
arch support (LWAS), valgus knee brace (VKB), and
valgus knee brace with lateral-wedged insole with
arch support (VKB+LWAS). The FI group acted
as a control during gait analysis to mimic normal
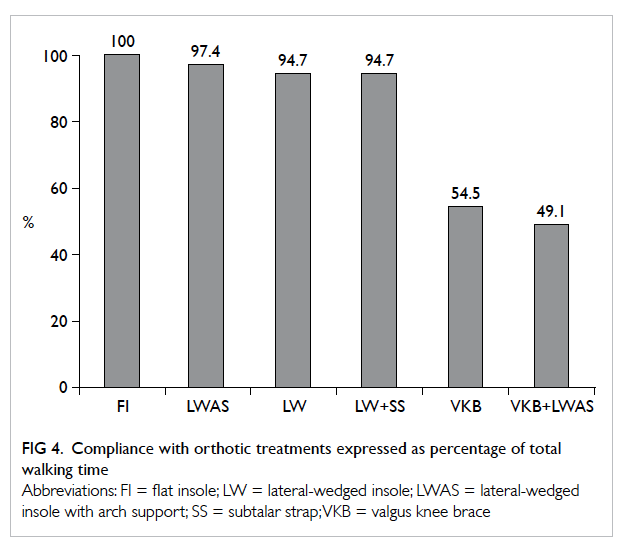
walking. The designs of the orthotics are shown
in Figure 1. The insoles were custom-made in the
Department of Prosthetics and Orthotics at Queen
Mary Hospital, while the Unloader valgus knee
braces (Össur hf, Reykjavik, Iceland) were ordered
for each patient after measurement. Each of the
orthotic treatments was prescribed for 4 weeks and
each patient underwent 24 weeks of treatment to use
all six orthotics.
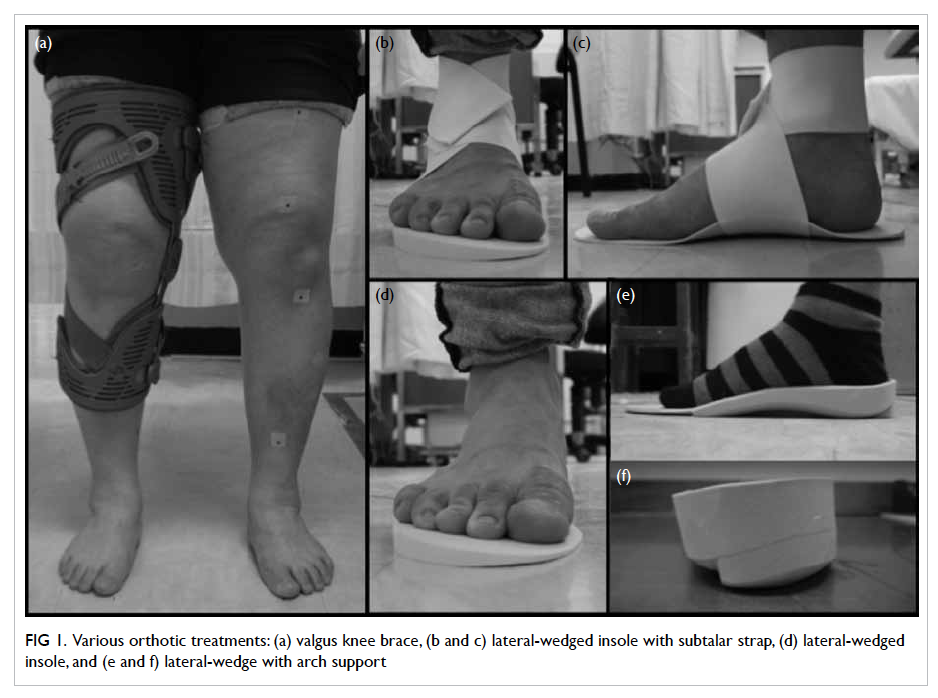
Figure 1. Various orthotic treatments: (a) valgus knee brace, (b and c) lateral-wedged insole with subtalar strap, (d) lateral-wedged insole, and (e and f) lateral-wedge with arch support
For subjective clinical outcomes, pain scores
using the visual analogue scale (VAS) and version
3.1 of the Chinese-validated Western Ontario and
McMaster Universities Arthritis Index (WOMAC)
were measured. The VAS, with a scale from 0 to 10,
was used purely for pain severity. The WOMAC
score was ascertained by a self-administered
questionnaire consisting of 24 items and subdivided
into three categories: pain (5 items), stiffness (2
items), and difficulty performing daily activities (17
items). Analgesic use (number of times required per
week) was also compared. Pretreatment and interval
assessments were completed after each orthotic
treatment. Paired t test was used for analysis.
Gait analysis
Three-dimensional gait analyses were performed
for each patient both before and during use of each
orthotic treatment at the gait laboratory at the
Duchess of Kent Children’s Hospital, Hong Kong,
which is an affiliated hospital within the same cluster
as Queen Mary Hospital.
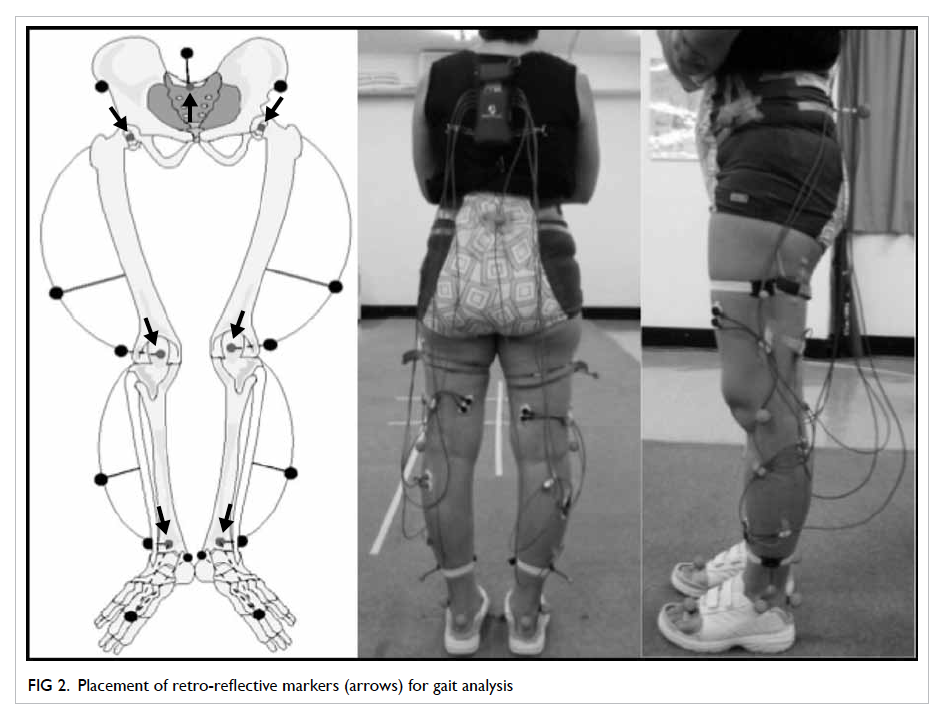
Fifteen retro-reflective markers were placed
according to the Plug in Gait model (Vicon Industries,
Inc, Edgewood [NY], US) as shown in Figure 2.
The markers were placed at the bilateral anterior
superior iliac spines, midway between the posterior
superior iliac spine, lateral epicondyle of the knee,
lateral lower third of the thigh, lateral malleolus,
lower third of the shin, second metatarsal head, and
calcaneus at the level of the second metatarsal head.
Three-dimensional positions of the markers and
kinematic data were collected by six cameras using
the 370 motion analysis system (Vicon Industries,
Inc) at a sampling frequency of 60 Hz. Kinetic data
were collected using the 370 motion analysis system
synchronised with a multicomponent force platform
(Kistler, Winterthur, Switzerland) at 60 Hz.
Peak and mean KAMs during the stance
phase of the gait cycle were measured. Mechanical
alignment throughout the gait cycle was derived
from the hip centre, knee centre, and ankle centre
from the retro-reflective markers. After data
collection from the gait analysis laboratory, data
were analysed jointly by orthopaedic surgeons
and prosthetic and orthotic specialists who had a
background in biomedical engineering. Gait analysis
comparison was made with the FI group and baseline
control data. An assumption was made that the flat insole would not alter the knee kinematics. The
control data from the gait laboratory consisted of 47
aged-matched healthy participants with normal gait
pattern.
Paired t tests were used for comparison of
different gait parameters between the orthotic type
and baseline measurement.
Results
Eighteen patients (36 knees) were initially recruited
into our study. Nineteen knees of 10 patients
completed the study, and the remaining eight patients
withdrew for personal reasons. Of the 10 patients,
nine had bilateral disease and one had unilateral
disease. Ten knees were right knees and nine were
left knees. There were six women and four men. The
mean age of the patients was 56 years (range, 51-65
years). The pretreatment motion arc ranged from 65°
to 140° (mean, 122°).
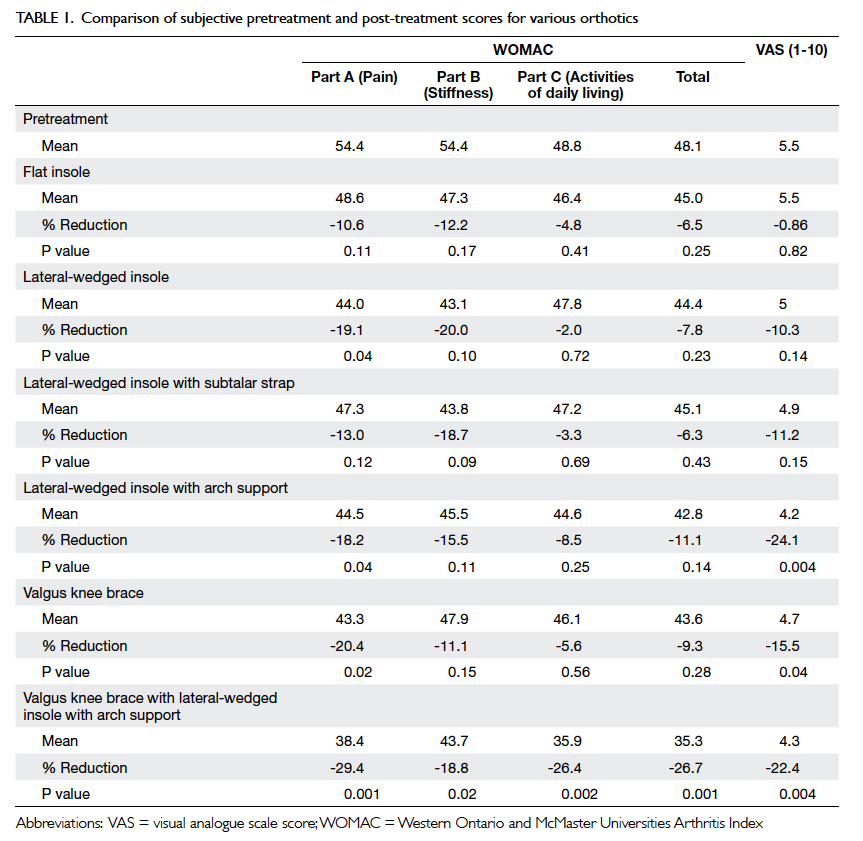
The changes in mean WOMAC and VAS scores
for various orthotic treatments and their comparison
with pretreatment scores are shown in Table 1. The
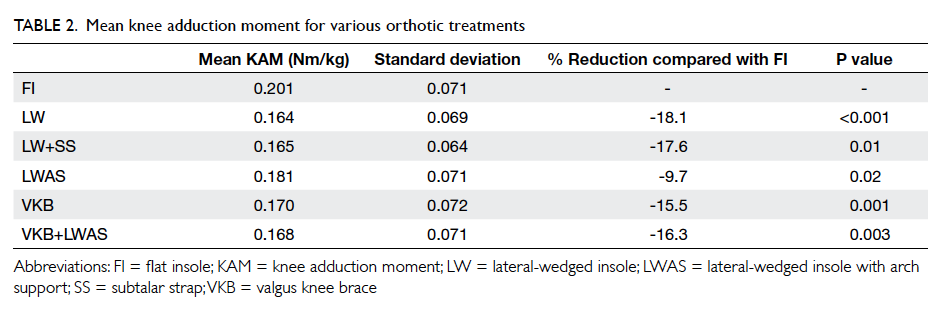
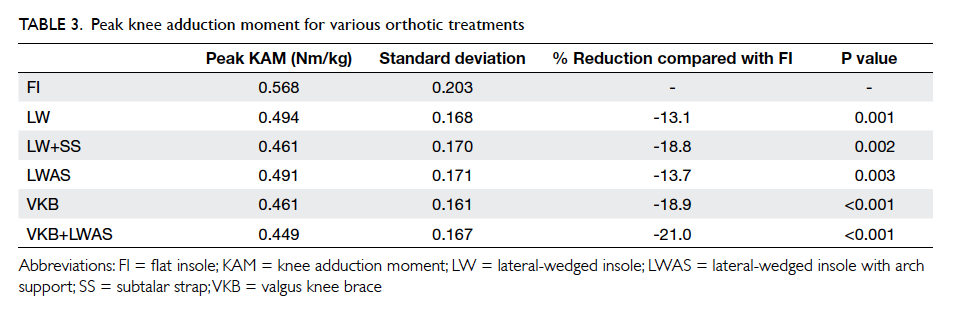
results of mean and peak KAMs throughout the gait
cycle with different orthotics are shown in Figure
3a. The mean and peak KAMs for each orthotic are
shown in Tables 2 and 3, respectively. Figure 3b shows
the knee mechanical alignment derived from the hip
centre, knee centre, and ankle centre. The initial 65%
of the gait cycle represents the stance phase and the
later 35% is the swing phase. Compliance with the
orthotic treatments is shown in Figure 4.
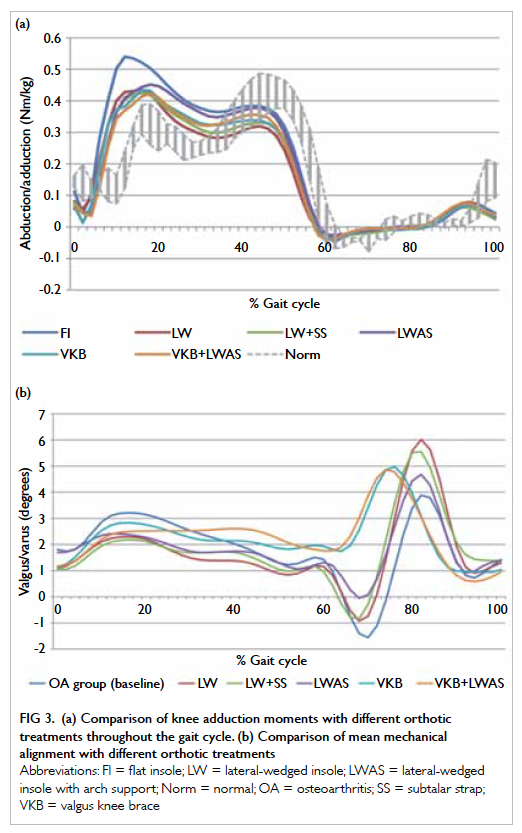
Figure 3. (a) Comparison of knee adduction moments with different orthotic treatments throughout the gait cycle. (b) Comparison of mean mechanical alignment with different orthotic treatments
The LW group demonstrated a significant
reduction of 19.1% in the WOMAC pain score (P=0.04). Reductions in total and other
WOMAC subscale scores, VAS score, and analgesic
requirement were observed, but none were
statistically significant. Mean and peak KAMs were
reduced by 18.1% and 13.1% (P<0.05), respectively,
when compared with the FI group. The compliance
rate was 94.7% of total walking time.
With the addition of subtalar strapping in the
hope of increasing the effectiveness of the lateral
wedge, the LW+SS group demonstrated a greater
reduction of peak KAM (18.8%), but a smaller degree
of reduction in mean KAM (17.6%) [P<0.05]. The
net effect of LW+SS did not confer any statistically
significant reduction in VAS score, WOMAC score,
or analgesic requirement when compared with the
pretreatment scores. The compliance rate for the
LW+SS group was 94.7% of total walking time.
The LWAS group demonstrated statistically
significant reduction in VAS score of 24.1% (P=0.004)
and WOMAC pain score of 18.2% (P=0.04).
Mean and peak KAMs were also significantly
reduced by 9.7% and 13.7%, respectively (P<0.05).
The degree of reduction in VAS score was greatest in
the LWAS group when compared with the LW and
LW+SS groups. Score of VAS may be a more reliable
predictor of actual symptom improvement than the
WOMAC pain score. The compliance
rate was also greatest for the LWAS group at 97.4%
of total walking time. No significant difference in
analgesic requirement was observed.
With respect to mean mechanical alignment,
as shown in Figure 3b, all the insole groups (LW,
LW+SS, and LWAS) showed lower varus angle
throughout the stance phase. The stance phase is the
symptomatic phase when the knee is under loading.
The VKB group showed a statistically
significant reduction in VAS score and WOMAC
pain score of 15.5% (P=0.04) and 20.4% (P=0.02),
respectively. The WOMAC total score and other subscale scores showed some reductions, but
these were not statistically significant. The analgesic
requirement was also significantly reduced from
1.5 days/week pretreatment to 0.5 days/week post-treatment
(P=0.04). Mean and peak KAMs were
reduced by 15.5% and 18.9%, respectively (P<0.05).
Mechanical alignment, as seen in Figure 3b, showed
reduced varus angulation during the early stance
phase. The interval between 15% and 20% of the
gait cycle, representing the heel strike to mid-stance
phase, was shown to have reduced the varus angle
when compared with baseline. The varus angle
remained constant throughout the stance phase,
which was related to restricted motion of the knee
inside the brace. Compliance was significantly lower
than that for any of the insole groups at 54.5% of
the total walking time. The low compliance rate was
likely due to the bulky size of the valgus knee brace causing skin discomfort, especially in the hot and
humid climate in this region.
The LWAS seemed to be the best insole
treatment for pain relief and improvement in VAS
score, so we further evaluated the combination
effects of the VKB and LWAS treatments. Additive
effects were observed with combined treatment. The
VKB+LWAS group showed significant reductions
in VAS score, as well as WOMAC total and all subscale scores. Score of VAS reduced by 22.4% (P=0.004),
WOMAC pain score reduced by 29.4% (P=0.001),
WOMAC stiffness score reduced by 18.8% (P=0.02),
WOMAC activities of daily living score reduced by
26.4% (P=0.002), and WOMAC total score reduced
by 26.7% (P=0.001). The extent of reduction in the
WOMAC total and subscale scores for this group was
the greatest of the treatment groups. The analgesic
requirement was also significantly reduced from
1.5 days/week pretreatment to 0.6 days/week post-treatment
(P=0.04). Peak KAM showed the greatest
reduction of all the orthotic groups of 21.0%, while
mean KAM showed moderate reduction of 16.3%
(P<0.05). With regard to the mechanical alignment,
reduction in varus angle was observed in the early
stance phase, as in the isolated VKB group. The
compliance, as expected, was lowest among all the
treatment arms with only 49.1% of total walking
time.
Discussion
The current literature recommendations for
orthotic treatment for medial compartment knee
osteoarthritis are still varied. In a guideline by
the Osteoarthritis Research Society International
(OARSI), insoles were concluded to be of benefit
to reduce pain and improve ambulation in knee
osteoarthritis.17 However, in another guideline by
the American Academy of Orthopaedic Surgeons
(AAOS), it was concluded that lateral-wedged insoles could not be suggested for patients with
symptomatic osteoarthritis.18 Lateral-wedged
insoles have been shown to correct the femorotibial
angle19 and reduce the peak external KAM.12 20 Toda et al21 were able to demonstrate a dose-response
correction of the femorotibial angle using insoles
with different elevations. The effect on subjective
scores showed significant improvements in some,22
but not all studies.23 24 Two randomised controlled
trials by Maillefert et al23 and Baker et al24 did not
show statistically significant changes in WOMAC
scores with lateral-wedged insoles, although there
was a significant reduction in non-steroidal anti-inflammatory
drug intake in the insole group.
Our results showed reduction in WOMAC
pain score with LW and LWAS, but more
importantly, a greater percentage reduction in VAS
score with LWAS. Addition of subtalar strapping to lateral-wedged insoles was shown in other studies to
improve VAS scores, and decrease the femorotibial
angle25 and peak KAM26 when compared with a lateral-wedged insole alone. The potential drawbacks
of subtalar strapping include increased sole pain.27
The results from our study did not demonstrate the
additional benefit with subtalar strapping in terms of
WOMAC score or mean KAM. With a significantly
greater reduction in VAS with LWAS than LW (24.1%
vs 10.3%) and a high compliance rate, we believe
LWAS is the insole of choice and can be offered to
patients with early isolated medial compartment
knee osteoarthritis.
Knee bracing acts by inducing a valgus force
by the three-point bending principle. The OARSI
guideline suggests that knee bracing could reduce
pain, improve stability, and reduce the risk of fall
in patients with mild-to-moderate osteoarthritis
or valgus instability.17 However, the guideline from
the AAOS could not conclude for or against the
use of valgus-directed bracing.18 Advantages of
knee bracing include avoidance of surgery and
the potential surgical complications, while the
disadvantages include compliance and the cost of
manufacturing the brace.28 A randomised controlled
trial by Brouwer et al29 compared three treatment
groups of valgus knee brace plus medical treatment,
insole plus medical treatment, and medical treatment
alone. The brace plus medical treatment was shown
to have borderline benefit compared to medical
treatment alone in terms of pain score and function.29
These findings concur with our study result of
improved WOMAC pain subscale score and reduced
analgesic requirement with valgus knee brace when
compared to pretreatment scores. From the kinetics
perspective, Pollo et al7 were able to demonstrate
reduction in net external KAM by 13%. Our gait
analysis model was able to reproduce reduction in
mean KAM by 18.9%. Despite the potential benefits
from valgus knee brace, compliance remains a major
drawback. With a compliance rate of 54.5%, many
of our patients claimed that they did not wear the
braces outdoors due to skin discomfort in the hot
and humid climate. Our evidence would suggest
valgus knee brace is suitable for selected patients
with mild knee osteoarthritis, with consideration of
the problem with fitting and compliance.
Our current study was among the few to
evaluate the effects of combination orthotic
treatment with valgus knee brace and lateral-wedged insole with arch support. The
VKB+LWAS group was the only one to demonstrate
significant reductions in WOMAC total and all subscale scores, analgesic use, and KAM when
compared with pretreatment. These results further
reiterate the dose-response relationship in reducing
KAM to achieve improvement in objective knee
scores. Despite these findings, the poor compliance
rate would render this orthotic treatment less
advisable.
Limitations
Limitations of our study included a small sample
size, selection bias, self-selection bias, and a short
follow-up period. Similar studies of less than 20
patients are seen in many studies of gait analysis.30 31 32 A larger sample size would provide a higher power
to determine the statistical significance in more of
the evaluated parameters. Compliance with orthotic
treatment, in particular with the valgus knee brace,
was another concern. Confounding factors in our
study included the frequency of weight-bearing
activities, which could be difficult to quantify.
This was a cross-over study, with all patients
having to be treated sequentially with all six
orthotic combinations. The advantages are an
economy of sample size without the need to
account for heterogeneity of the patient groups.
The disadvantages of the design include lack of a
treatment break and lack of randomisation in the
treatment sequence. Scores of VAS reported by
elderly people may also be inaccurate.
Conclusions
Knee osteoarthritis continues to pose a significant
burden to our community with its ageing population
and increased incidence of obesity. While operative
treatments are not without risk, orthotic treatment
also has its advantages and disadvantages. Our
current study was able to demonstrate from subjective
scores and gait analysis that orthotic treatment can
alter knee loading and alleviate symptoms. The lateral-wedged insole with arch support is optimal,
while valgus knee brace is equally effective, with fair
compliance. Further studies with a larger sample size
are required to evaluate the effectiveness in the long
term.
References
1. Knutson K, Lindstrand A, Lidgren L. Survival of knee
arthroplasties. A nation-wide multicentre investigation of
8000 cases. J Bone Joint Surg Br 1986;68:795-803.
2. Swedish Knee Arthroplasty Registry. SKAR Annual
Report; 2011.
3. Ledingham J, Regan M, Jones A, Doherty M. Radiographic
patterns and associations of osteoarthritis of the knee in
patients referred to hospital. Ann Rheum Dis 1993;52:520-6. Crossref
4. Sharma L, Song J, Dunlop D, et al. Varus and valgus
alignment and incident and progressive knee osteoarthritis.
Ann Rheum Dis 2010;69:1940-5. Crossref
5. Chang A, Hayes K, Dunlop D, et al. Thrust during
ambulation and the progression of knee osteoarthritis.
Arthritis Rheum 2004;50:3897-903. Crossref
6. Birmingham TB, Hunt MA, Jones IC, Jenkyn TR, Giffin JR.
Test-retest reliability of the peak knee adduction moment
during walking in patients with medial compartment knee
osteoarthritis. Arthritis Rheum 2007;57:1012-7. Crossref
7. Pollo FE, Otis JC, Backus SI, Warren RF, Wickiewicz TL.
Reduction of medial compartment loads with valgus
bracing of the osteoarthritic knee. Am J Sports Med
2002;30:414-21.
8. Lindenfeld TN, Hewett TE, Andriacchi TP. Joint loading
with valgus bracing in patients with varus gonarthrosis.
Clin Orthop Relat Res 1997;344:290-7. Crossref
9. Pagani CH, Böhle C, Potthast W, Brüggemann GP. Short-term
effects of a dedicated knee orthosis on knee adduction
moment, pain, and function in patients with osteoarthritis.
Arch Phys Med Rehabil 2010;91:1936-41. Crossref
10. Toriyama M, Deie M, Shimada N, et al. Effects of unloading
bracing on knee and hip joints for patients with medial
compartment knee osteoarthritis. Clin Biomech (Bristol,
Avon) 2011;26:497-503. Crossref
11. Hinman RS, Bowles KA, Bennell KL. Laterally wedged
insoles in knee osteoarthritis: do biomechanical effects
decline after one month of wear? BMC Musculoskelet
Disord 2009;10:146. Crossref
12. Fantini Pagani CH, Hinrichs M, Brüggemann GP. Kinetic
and kinematic changes with the use of valgus knee brace
and lateral wedge insoles in patients with medial knee
osteoarthritis. J Orthop Res 2012;30:1125-32. Crossref
13. Butler RJ, Marchesi S, Royer T, Davis IS. The effect
of a subject-specific amount of lateral wedge on knee
mechanics in patients with medial knee osteoarthritis. J
Orthop Res 2007;25:1121-7. Crossref
14. Kakihana W, Akai M, Nakazawa K, Naito K, Torii S.
Inconsistent knee varus moment reduction caused by
a lateral wedge in knee osteoarthritis. Am J Phys Med
Rehabil 2007;86:446-54. Crossref
15. Belo JN, Berger MY, Koes BW, Bierma-Zeinstra SM. The
prognostic value of the clinical ACR classification criteria
of knee osteoarthritis for persisting knee complaints and
increase of disability in general practice. Osteoarthritis
Cartilage 2009;17:1288-92. Crossref
16. Kellgren JH, Lawrence JS. Radiological assessment of
osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. Crossref
17. Zhang W, Moskowitz RW, Nuki G, et al. OARSI
recommendations for the management of hip and
knee osteoarthritis, Part II: OARSI evidence-based,
expert consensus guidelines. Osteoarthritis Cartilage
2008;16:137-62. Crossref
18. Jevsevar DS, Brown GA, Jones DL, et al. The American
Academy of Orthopaedic Surgeons evidence-based
guideline on: treatment of osteoarthritis of the knee, 2nd
edition. J Bone Joint Surg Am 2013;95:1885-6.
19. Yasuda K, Sasaki T. The mechanics of treatment of the
osteoarthritic knee with a wedged insole. Clin Orthop
Relat Res 1987;215:162-72.
20. Shimada S, Kobayashi S, Wada M, et al. Effects of disease
severity on response to lateral wedged shoe insole for
medial compartment knee osteoarthritis. Arch Phys Med
Rehabil 2006;87:1436-41. Crossref
21. Toda Y, Tsukimura N, Kato A. The effects of different
elevations of laterally wedged insoles with subtalar
strapping on medial compartment osteoarthritis of the
knee. Arch Phys Med Rehabil 2004;85:673-7. Crossref
22. Sasaki T, Yasuda K. Clinical evaluation of the treatment of
osteoarthritic knees using a newly designed wedged insole.
Clin Orthop Relat Res 1987;221:181-7.
23. Maillefert JF, Hudry C, Baron G, et al. Laterally elevated
wedged insoles in the treatment of medial knee
osteoarthritis: a prospective randomized controlled study.
Osteoarthritis Cartilage 2001;9:738-45. Crossref
24. Baker K, Goggins J, Xie H, et al. A randomized crossover
trial of a wedged insole for treatment of knee osteoarthritis.
Arthritis Rheum 2007;56:1198-203. Crossref
25. Toda Y, Tsukimura N. A six-month followup of a
randomized trial comparing the efficacy of a lateral-wedge
insole with subtalar strapping and an in-shoe lateral-wedge
insole in patients with varus deformity osteoarthritis of the
knee. Arthritis Rheum 2004;50:3129-36. Crossref
26. Kuroyanagi Y, Nagura T, Matsumoto H, et al. The lateral
wedged insole with subtalar strapping significantly reduces
dynamic knee load in the medial compartment gait analysis
on patients with medial knee osteoarthritis. Osteoarthritis
Cartilage 2007;15:932-6. Crossref
27. Brouwer RW, Jakma TS, Verhagen AP, Verhaar JA,
Bierma-Zeinstra SM. Braces and orthoses for treating
osteoarthritis of the knee. Cochrane Database Syst Rev
2005;(1):CD004020.
28. Hanypsiak BT, Shaffer BS. Nonoperative treatment of
unicompartmental arthritis of the knee. Orthop Clin
North Am 2005;36:401-11. Crossref
29. Brouwer RW, van Raaij TM, Verhaar JA, Coene LN,
Bierma-Zeinstra SM. Brace treatment for osteoarthritis
of the knee: a prospective randomized multi-centre trial.
Osteoarthritis Cartilage 2006;14:777-83. Crossref
30. Foroughi N, Smith RM, Lange AK, Baker MK, Fiatarone
Singh MA, Vanwanseele B. Dynamic alignment and its
association with knee adduction moment in medial knee
osteoarthritis. Knee 2010;17:210-6. Crossref
31. van den Noort JJ, van der Esch M, Steultjens MP, et al.
Ambulatory measurement of the knee adduction moment
in patients with osteoarthritis of the knee. J Biomech
2013;46:43-9. Crossref
32. Kutzner I, Trepczynski A, Heller MO, Bergmann G. Knee
adduction moment and medial contact force—facts about
their correlation during gait. PLoS One 2013;8:e81036. Crossref