Hong Kong Med J 2015 Feb;21(1):23–9 | Epub 30 Jan 2015
DOI: 10.12809/hkmj144266
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Predictive factors for colonoscopy complications
Annie OO Chan, MB, BS, MD1; Louis NW Lee, MB, BS, FRCS (Edin)2; Angus CW Chan, MB, ChB, MD2; WN Ho, BHSs (Nursing)2; Queenie WL Chan, BHSs (Nursing)3; Silvia Lau, MPH, MSc4; Joseph WT Chan, MB, BS, FRCOG5
1 Gastroenterology & Hepatology Centre, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
2 Endoscopy Centre, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
3 Nursing Administration Department, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
4 Medical Physics & Research Department, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
5 Hospital Administration Department, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
Corresponding author: Dr Queenie WL Chan (wlchan@hksh.com)
Abstract
Objective: To determine factors predicting
complications caused by colonoscopy.
Design: Prospective cohort study.
Setting: A private hospital in Hong Kong.
Patients: All patients undergoing colonoscopy in
the Endoscopy Centre of the Hong Kong Sanatorium
& Hospital from 1 June 2011 to 31 May 2012 were
included. Immediate complications were those that
were recorded by nurses during and up to the day
after the examination, while delayed complications
were gathered 30 days after the procedure by
way of consented telephone interview by trained
student nurses. Data were presented as frequency
and percentage for categorical variables. Logistic
regression was used to fit models for immediate and
systemic complications with related factors.
Results: A total of 6196 patients (mean age, 53.7
years; standard deviation, 12.7 years; 3143 women)
were enrolled and 3657 telephone interviews
were completed. The incidence of immediate
complications was 15.3 per 1000 procedures
(95% confidence interval, 12.3-18.4); 50.5% were
colonoscopy-related, including one perforation
and other minor presentations. Being female (odds
ratioadjusted=1.6), use of monitored anaesthetic care
(odds ratioadjusted=1.8), inadequate bowel preparation
(odds ratioadjusted=3.5), and incomplete colonoscopy
(odds ratioadjusted=4.5) were predictors of risk for all
immediate complications (all predictors had P<0.05
by logistic regression). The incidence of delayed
complications was 1.6 per 1000 procedures (95%
confidence interval, 0.3-3.0), which comprised
five post-polypectomy bleeds and one post-polypectomy
inflammation. The overall incidence
of complications was 17.8 per 1000 procedures (95%
confidence interval, 13.5-22.1). The incidences of
complications were among the lower ranges across
studies worldwide.
Conclusion: Inadequate bowel preparation and
incomplete colonoscopy were identified as factors
that increased the risk for colonoscopy-related
complications. Colonoscopy-related complications
occurred as often as systemic complications,
showing the importance of monitoring.
New knowledge added by this
study
- The risks of local and systemic complications of colonoscopy are of paramount importance.
- Enforcing bowel preparation and post-polypectomy care may reduce the risk of delayed complications.
Introduction
Colonoscopy is an efficient, invasive, and
commonly used diagnostic tool with promising
therapeutic capacity. Common colonoscopy-related
complications include prolonged pain
and distension, and rarely draw medical attention
or lead to hospitalisation. Severe complications,
including bleeding and perforation, are potentially
life-threatening and require urgent management.
Although death is uncommon, occurring in no
more than 3 per 10 000 procedures, the incidence
of post-polypectomy bleeding and perforation
ranges from 1.6 to 14.8 and 0.2 to 1.0 per 1000
procedures, respectively.1 2 3 4 5 6 It is difficult to
accurately benchmark direct colonoscopy-related
complications due to the different outcome
measure definitions used in studies. For example,
some studies include immediate complications only,
while others extend the complication period to 7 or
30 days, and some studies include an extensive list
of complications while others include only bleeding
and perforation.1 2 5 7 8 9 10 Furthermore, the efficacy and
safety of the procedure vary across clinical settings
and the targeted populations. With no available local
data, consensus for complication incidence remains
inconclusive.
Intravenous sedation is routinely used during
colonoscopy to minimise the discomfort and pain
associated with the procedure. Endoscopists are
equipped to give sedatives and to monitor their
side-effects, but anaesthetists are often invited
to provide monitored anaesthetic care (MAC)
when the patient is considered to be at high risk
for complications, for instance, older patients and
those with multiple co-morbidities are particularly
vulnerable to complications. Systemic complications
vary from prolonged drowsiness to fatal events
such as cardiovascular or cerebrovascular events.
Cardiovascular events following sedation, such
as hypotension and myocardial infarction, during
colonoscopy have been reported to range from
0.1 to 59.1 per 1000 procedures. Cerebrovascular
events such as stroke range from 0.1 to 1.3 per 1000
procedures.3 6 10 The outcome variables are highly
heterogeneous, for example, Nelson et al’s study3
included myocardial infarction, vasovagal event, and
arrhythmia in the cardiovascular incidents, while
Ma et al’s study10 recorded hypotension only.10 Some
endoscopists opted to study complications related
to the use of carbon dioxide (CO2) insufflation and
absence of sedative use.11 12 13 This study aimed to record all complications systematically and to
determine the relevant risk factors.
Methods
This prospective study collected data for all
colonoscopies done from 1 June 2011 to 31
May 2012 at the Endoscopy Centre of the Hong
Kong Sanatorium & Hospital (HKSH), which is a private hospital in Hong Kong. Prior to
colonoscopy, patients were invited to give their
written consent for their participation in the study,
including for the 30-day follow-up telephone
interview. The Hospital Management Committee
involving the Research Ethics Committee of the
HKSH approved the study.
The complications were recorded by nurses
on a standard form during and immediately after
the procedure. The standard audit forms for
immediate and delayed colonoscopy complications
were designed by a research doctor, with the most
common complications based on literature review.
The immediate complications audit form
included patients’ demographics, use of sedation/analgesic/antispasmodic, use of MAC, gross
indications for colonoscopy (therapeutic or
diagnostic), type of therapeutic procedures
performed such as polypectomy, the reason for
incomplete colonoscopy (caecum intubation
failure), quality of bowel preparation (adequate –
good/adequate or not – fair/poor, which was rated
by the endoscopist), and the use of CO2 insufflation.
Complication data were divided into systemic and
colonoscopy-related complications. For systemic
complications, we captured data for nausea/vomiting, hypotension (systolic blood pressure
<100 mm Hg), bradycardia/tachycardia (heart rate
<50 to >100 beats/min), vasovagal fainting, and
other cardiovascular or cerebrovascular events.
For colonoscopy-related complications, data for
perforation, persistent pain/discomfort, abdominal
distension, and haemorrhage were gathered.
Delayed complications were defined as the
above events happening from the day after the
initial colonoscopy to the 30th day that required
readmission or admission to other hospitals. For
those readmissions, we automatically inspected
the records for the reasons and interventions if the
readmissions were complication-related. Otherwise,
trained student nurses or a research doctor
telephoned all consented participants to interview
for the 30-day complications using the delayed
complication audit form. A participant was declared
lost to follow-up after three telephone attempts. The
student nurses were trained by senior nurses and the
research doctor with standard instructions.
Data analysis was performed by the Statistical
Package for the Social Sciences (Windows version
14.0; SPSS Inc, Chicago [IL], US). Descriptive
statistics (mean, percentage, incidence, and/or 95% confidence interval [CI]) were used to
display the characteristics of the sample. For those
complications with zero events, only 95% CIs were
given.14 Backward logistic regression analyses were
performed to draw prediction models for immediate
complications, including colonoscopy-related
complications or systemic complications, and overall
complications, including immediate and delayed
complications, from the sample; entering variables
were chosen from age, sex (male or female), use of
MAC (yes or no), sufficiency of bowel preparation
(adequate or not), and completion of colonoscopy
(yes or no) according to the results of the univariate
analyses by Pearson Chi squared tests of all potential
independent variables, with a significance level set
at 10%; variable inclusion in the iteration was set
at P<0.1 for backward logistic regression analyses.
Returning coefficients of the variables were
interpreted as adjusted odds ratio (ORadjusted) with
95% CI provided. All significance levels were set at
two-sided α=0.05.
Results
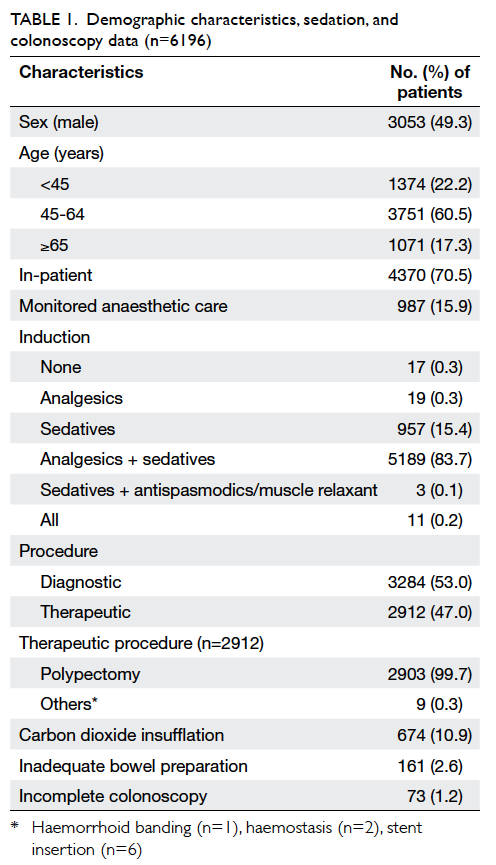
A total of 6196 colonoscopies (3143 women; mean
age 53.7 years; standard deviation, 12.7 years) were
done during the study period. Most patients were
aged between 45 and 64 years, were in-patients, had
undergone diagnostic colonoscopy, and received
intravenous sedation (60.5%, 70.5%, 53.0%, and
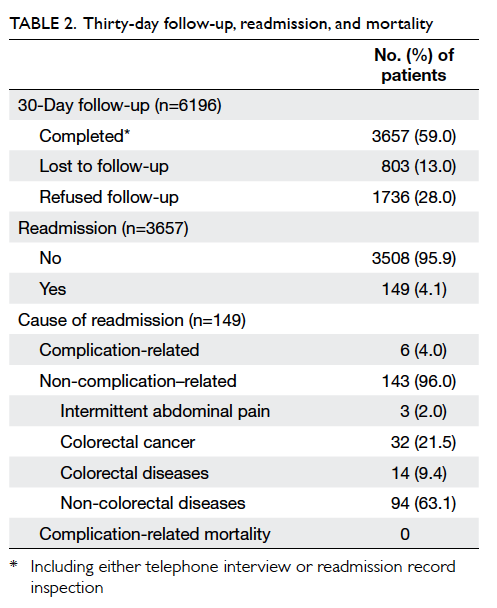
99.4% respectively; Table 1). The data for immediate
complications were complete, while the 30-day
follow-up was completed for 3657 procedures (803
were lost to follow-up and 1736 refused; compliance
rate 59.0%; Table 2).
Of the 6196 colonoscopies, 2912 were
therapeutic with 99.7% dedicated to polypectomy
(Table 1). There were 73 (1.2%) cases of incomplete
colonoscopy, 18 (24.7%) of which were due
to inadequate preparation. Other reasons for
incomplete colonoscopy were tumour obstruction
(15 of 73; 20.5%) and intention of sigmoidoscopy
or stent insertion (26 of 73; 35.6%). A total of 149
patients were readmitted within 30 days after
the procedure, of which six (4.0%) were related
to complications. The other reasons were cancer,
gastro-intestinal disease, or cardiac events (Table 2).
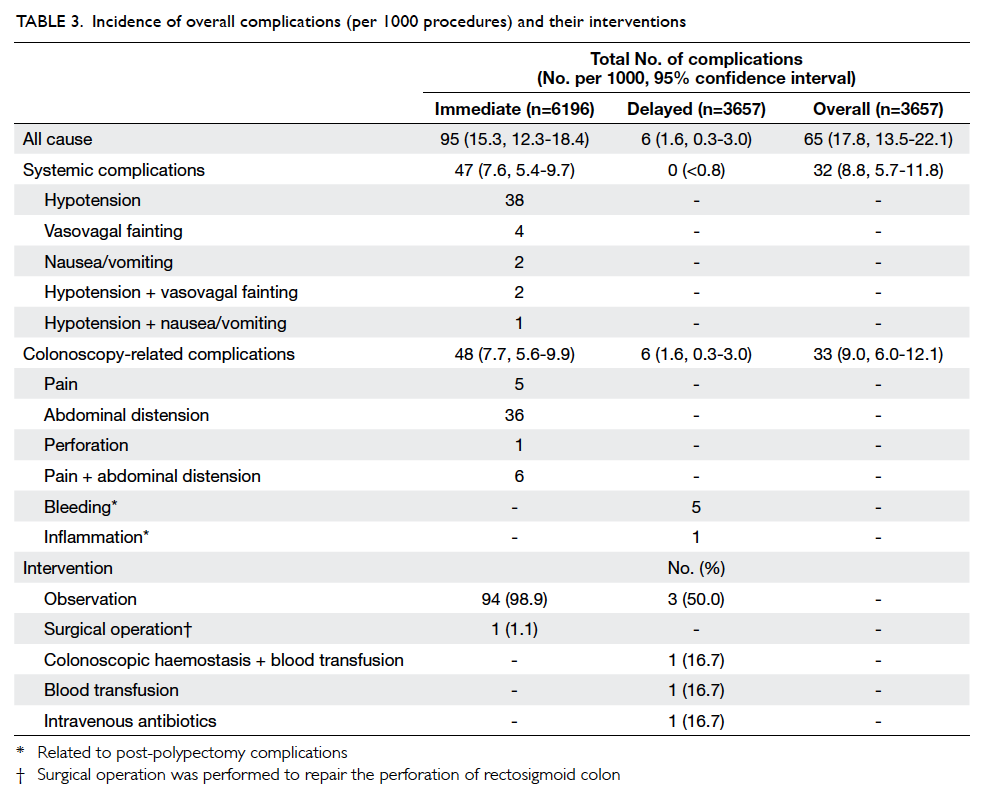
Systemic complications
Regarding the choice of sedation, midazolam and
pethidine were the most used at 81.5% and 82.0%,
respectively, while 15.9% of patients underwent
MAC. Immediate complications reported included
hypotension, vasovagal fainting, and nausea/vomiting, or a combination (6.1, 0.6, 0.3, and 0.5
per 1000 procedures, respectively; Table 3). There
were no severe cardiovascular events such as
heartbeat irregularity or myocardial infarction or
cerebrovascular events such as stroke. Furthermore,
none of the patients reported delayed systemic
complications in the 30-day follow-up.
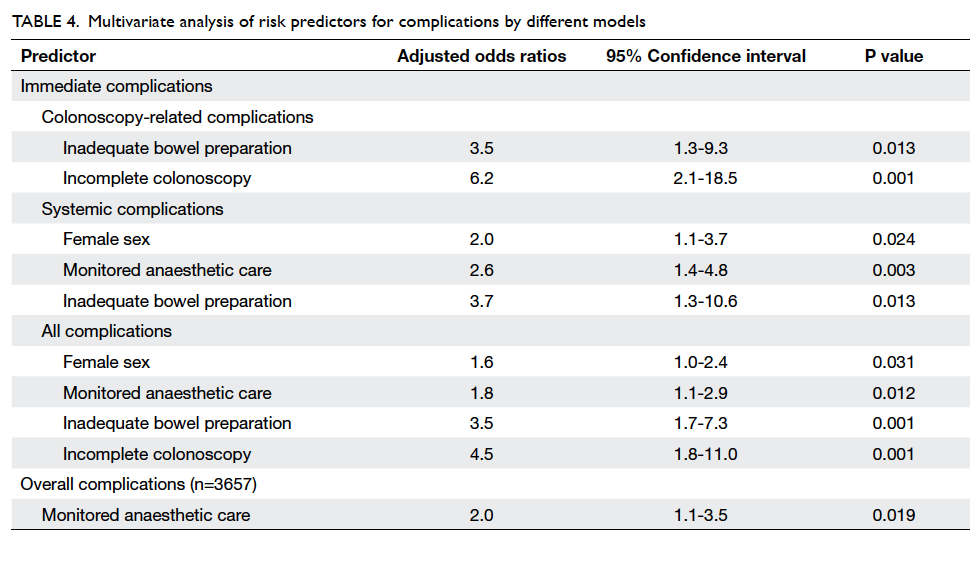
Modelling to study the potential risk factors
showed that being female, use of MAC, and
inadequate bowel preparation were the significant
independent predictors for systemic immediate
complications (ORadjusted=2.0, 2.6, and 3.7,
respectively; all were P<0.05; Table 4).
Colonoscopy-related complications
Immediate colonoscopy-related complications were
recorded for 48 patients (7.7 per 1000 procedures),
including extensive pain/discomfort, abdominal
distension, and perforation (Table 3). The only
perforation was at the sigmoid-rectal junction and
was due to adhesion, which might be related to
previous abdominal surgery (total hysterectomy and
bilateral salpingo-oophorectomy was done 10 years
previously). In the 30-day follow-up, six patients
reported complication-related readmissions, five
of whom were for bleeding after discharge from
hospital and one was for inflammation; all were
caused by polypectomy.
Modelling was done to formulate a predictive
algorithm for significant independent risk factors
and outcome events (Table 4). Inadequate bowel
preparation and incomplete colonoscopy were the
significant predictors for immediate colonoscopy-related
complications (ORadjusted=3.5 and 6.2,
respectively; both were P<0.05) and for all immediate
complications (ORadjusted=3.5 and 4.5, respectively;
both were P<0.05). In the model for all immediate
complications, being female and use of MAC were
also predictors (ORadjusted=1.6 and 1.8, respectively;
all were P<0.05).
A predictive model was also done for overall
complications, including all immediate and delayed
complications among those who completed follow-up
at 30 days. The effect of previous significant
predictors was transient in that they did not predict
the overall complications occurring in the 30-day
post-colonoscopy period. Monitored anaesthetic
care was the only predictor during the 30-day period
(ORadjusted=2.0; P=0.019).
Discussion
Significance of this study
Inadequate bowel preparation and incomplete
colonoscopy were identified as risk factors
for colonoscopy-related complications. Other
complications were mostly hypotension and
abdominal distension. No myocardial infarction,
transient ischaemic attack, or death relating to
colonoscopy was reported.
Contribution of individual characteristics to
the complications
Colonoscopy is rarely a complication-free
procedure, but a good understanding of the possible
complications can help to minimise them. While
experienced endoscopists, diagnostic procedures,
and young patients are protective factors for
colonoscopy complications, trainee endoscopists,
therapeutic procedures, advanced age, female
sex, obesity, co-morbidity, anticoagulant use, and
previous abdominal surgery are risk factors for
complications.3 5 6 10 15 16 17 The relatively low incidence
of complications recorded in this study could be
attributed to the fact that more than half of the
procedures were diagnostic, thus reducing the
potential for polypectomy-associated complications.
Other events—such as abdominal pain and
distension, hypotension, vasovagal fainting, and
nausea/vomiting—accounted for 98.9% of all
immediate complications; these events were mostly
reported by women (60.6%; ORadjusted=1.6; Table
4). This result is consistent with the literature.17
This effect could possibly be explained by different
perceptions of somato-sensation, which could be
traced back to the socio-emotional cultivation and
cultural expectation of the different sexes.18
Hidden factors that may contribute to
complications
Despite the sex effect, use of MAC, inadequate
bowel preparation, and incomplete colonoscopy
were all related to immediate complications. The use
of MAC, in particular, requires more interpretation
because it has not been found to be a risk factor
in other studies and its use ought not be a cause
of complications. However, MAC is designed for
patients who are vulnerable to the complications of
sedation and the procedure, especially those with co-morbidities
and who are at an advanced age. In this
study, co-morbidity was not reviewed, but patients
who underwent MAC were significantly older than
those who did not (mean age, 56.1 vs 53.3 years;
P<0.001, t test) which may be partly contributory.
However, age was not significantly associated
with any of the complications after adjustment for
other factors. Age might have a greater impact if co-morbidity
was also considered and this may be an
area for further study.
Inadequate bowel preparation, in which faeces
obscure the inner lining of the colon, impedes the
vision and heightens the risk for complications.
Likewise, incomplete colonoscopy due to inadequate
bowel preparation or unbearable discomfort
inevitably increases the risk for complications. These
results are consistent with other studies.2 3 10
A large proportion (59%) of the study
population completed the study. Per protocol
univariate analyses showed that use of MAC was the
sole significant factor related to overall complications
(Table 4).
Other factors
Sedation-free colonoscopy is a feasible alternative
that could reduce the risk of systemic complications;
use of CO2 insufflation might increase its tolerability
while maintaining visibility. In this study, a sedation-free
procedure was performed in only 36 patients,
with no complications; CO2 insufflation was done for
647 (10.9%) patients instead of gas (room air), with
only minor complications encountered (two patients
reported abdominal distension and seven reported
hypotension/vasovagal fainting). Insufflation with
CO2 could be adopted more widely because it is
non-explosive, absorbable, and does not affect the
mucosal blood flow, thus minimising discomfort
and the risk of colonic ischaemia. According to
Bretthauer et al,19 CO2 insufflation leads to quicker
recovery, and less pain and complications. These
advantages are supported by other studies including
local research.11 19 20 These factors might inspire
greater use of CO2 insufflation and minimise use of
sedation for selected patients.12 13 21
Inadequate bowel preparation not only
hampers completion of the procedure, but also
increases the risk for complications. As evidenced
from the prediction models, inadequate bowel
preparation significantly increases the occurrence
of complications. In addition to implementing the
current standardised bowel preparation protocol,
enforcement of patient education, compliance, and
early admission for monitored bowel preparation
might help to further suppress the rate for inadequate
bowel preparation.
Limitations
Many of the patients were lost to contact by
telephone. In this study, we assumed that the pattern
of missing patients was random and was not affected
by whether or not the patients had complications.
However, self-selection bias might exist. If patients
without complications were more likely to be lost
to contact, the rate of delayed complications would
be overestimated. However, the rate of delayed
complications would be underestimated if the
patients had been admitted to other hospitals or had
died.
Endoscopist experience, and patient characteristics of co-morbidities and
severe symptoms before the procedure were not recorded for analysis
in this study. These are potential risk factors for
complications.
In view of the importance of monitoring the
complications of colonoscopy, further study might
include the missing variables of co-morbidity,
endoscopist experience, symptoms at presentation and oxygen level, and explore factors such as the
influence of body mass index and medical history,
sedation dose, indication for colonoscopy, use of
laxatives and compliance, and post-colonoscopy
diagnosis/pathology that might help to minimise the
variance on prediction of complications.
Acknowledgements
We would like to thank Dr Sheri Lim, former
Administrative Officer (Medical) who proposed
and developed the audit. We are grateful to Dr KM
Lai, Head of Department of Anaesthesiology for his
expert advice on the anaesthetic terminology; Dr
Raymond Yung and Dr KN Lai, Assistant Medical
Superintendents for their valuable suggestions
and encouragement; Ms Grace Wong, Medical
Records Manager for coordinating with different
departments; and Ms Sara Fung, former Research
Nurse for coordinating the project. Also, thanks to all
doctors who contributed their knowledge and data,
for this study would not have been accomplished
without them.
References
1. Lorenzo-Zúñiga V, Moreno de Vega V, Doménech E,
Mañosa M, Planas R, Boix J. Endoscopist experience as a
risk factor for colonoscopic complications. Colorectal Dis
2010;12(10 Online):e273-7.
2. Gastrointestinal endoscopy, version 1. Australasian Clinical Indicator Report 2003-2010. Australian Council on Healthcare Standards; 2010.
3. Nelson DB, McQuaid KR, Bond JH, Lieberman DA, Weiss
DG, Johnston TK. Procedural success and complications
of large-scale screening colonoscopy. Gastrointest Endosc
2002;55:307-14. CrossRef
4. Rathgaber SW, Wick TM. Colonoscopy completion and
complication rates in a community gastroenterology
practice. Gastrointest Endosc 2006;64:556-62. CrossRef
5. Rabeneck L, Paszat LF, Hilsden RJ, et al. Bleeding and perforation after outpatient
colonoscopy and their risk factors in usual clinical practice.
Gastroenterology 2008;135:1899-1906, 1906.e1.
6. Viiala CH, Zimmerman M, Cullen DJ, Hoffman NE.
Complication rates of colonoscopy in an Australian
teaching hospital environment. Intern Med J 2003;33:355-9. CrossRef
7. Ko CW, Riffle S, Michaels L, et al. Serious complications within 30 days of screening
and surveillance colonoscopy are uncommon. Clin
Gastroenterol Hepatol 2010;8:166-73. CrossRef
8. Singh H, Penfold RB, DeCoster C, et al. Colonoscopy and its complications across
a Canadian regional health authority. Gastrointest Endosc
2009;69:665-71. CrossRef
9. Teruki O, Keiichi O. The safety of endoscopic day surgery
for colorectal polyps. Dig Endosc 2008;20:92-5. CrossRef
10. Ma WT, Mahadeva S, Kunanayagam S, Poi PJ, Goh KL.
Colonoscopy in elderly Asians: a prospective evaluation in
routine clinical practice. J Dig Dis 2007;8:77-81. CrossRef
11. Wong JC, Yau KK, Cheung HY, Wong DC, Chung CC,
Li MK. Towards painless colonoscopy: a randomized
controlled trial on carbon dioxide-insufflating colonoscopy.
ANZ J Surg 2008;78:871-4. CrossRef
12. Bayupurnama P, Nurdjanah S. The success rate of
unsedated colonoscopy examination in adult. Internet
Journal of Gastroenterology 2010;9:2.
13. Ylinen ER, Vehviläinen-Julkunen K, Pietilä AM, Hannila
ML, Heikkinen M. Medication-free colonoscopy—factors related to pain and its assessment. J Adv Nurs
2009;65:2597-607. CrossRef
14. Ho AK. When the numerator is zero: another lesson on
risk. Am Biol Teach 2009;71:531-3. CrossRef
15. Miller A, McGill D, Bassett ML. Anticoagulant therapy,
anti-platelet agents and gastrointestinal endoscopy. J
Gastroenterol Hepatol 1999;14:109-13. CrossRef
16. Dobbins C, DeFontgalland D, Duthie G, Wattchow DA. The
relationship of obesity to the complications of diverticular
disease. Colorectal Dis 2006;8:37-40. CrossRef
17. Ko CW, Riffle S, Shapiro JA, et al. Incidence of minor complications and time lost
from normal activities after screening or surveillance
colonoscopy. Gastrointest Endosc 2007;65:648-56. CrossRef
18. Kroenke K, Spitzer RL. Gender differences in the reporting
of physical and somatoform symptoms. Psychosom Med
1998;60:150-5. CrossRef
19. Bretthauer M, Lynge AB, Thiis-Evensen E, Hoff G, Fausa O,
Aabakken L. Carbon dioxide insufflation in colonoscopy:
safe and effective in sedated patients. Endoscopy
2005;37:706-9. CrossRef
20. Welchman S, Cochrane S, Minto G, Lewis S. Systematic
review: the use of nitrous oxide gas for lower gastrointestinal
endoscopy. Aliment Pharmacol Ther 2010;32:324-33. CrossRef
21. Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Sedation-free
colonoscopy. Dis Colon Rectum 2005;48:855-9. CrossRef
Find HKMJ in MEDLINE: