DOI: 10.12809/hkmj144235
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Chinese talismans as a source of lead exposure
CK Chan, Dip Clin Tox, FHKAM (Emergency Medicine)1; CK Ching, FRCPA, FHKAM (Pathology)2; FL Lau, FRCS (Edin), FHKAM (Emergency Medicine)1; HK Lee, MSc3
1 Hong Kong Poison Information Centre, United Christian Hospital, Kwun Tong, Hong Kong
2 Hospital Authority Toxicology Reference Laboratory, Princess Margaret
Hospital, Laichikok, Hong Kong
3 Department of Clinical Pathology, Tuen Mun Hospital, Tuen Mun, Hong
Kong
Corresponding author: Dr CK Chan (chanck3@ha.org.hk)
Abstract
We describe a case of lead exposure after prolonged
intake of ashes from burnt Chinese talismans. A
41-year-old woman presented with elevated blood
lead level during screening for treatable causes of
progressive weakness in her four limbs, clinically
compatible with motor neuron disease. The source of
lead exposure was confirmed to be Chinese talismans
obtained from a religious practitioner in China. The
patient was instructed to burn the Chinese talismans
to ashes, and ingest the ashes dissolved in water, daily
for about 1 month. Analysis of the Chinese talismans
revealed a lead concentration of 17 342 µg/g (ppm).
Case report
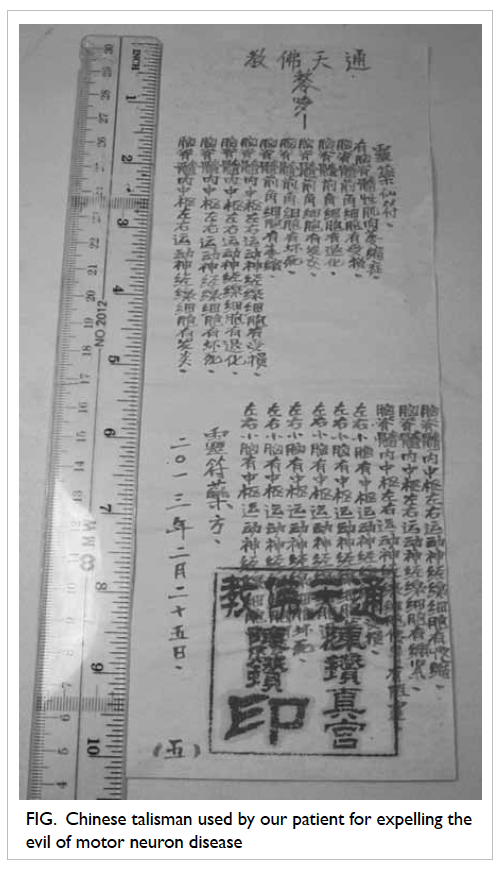
Chinese talisman is a religious handwriting or
calligraphy which is believed to possess magical
powers for expelling evils and avoiding misfortune.
It is usually obtained from Daoism religious
practitioners.1 Some people believe that consuming
burnt Chinese talisman ashes dissolved in water is
useful in curing diseases. Here we report a case of
lead exposure after prolonged intake of ashes from
burnt Chinese talismans.
The patient was a 41-year-old woman. She
presented with progressive weakness of four limbs
with signs of upper motor neuron disease (MND)
since March 2012. Electromyogram findings were
compatible with diffuse anterior horn cell disorder.
Motor neuron disease was clinically diagnosed by
the treating neurologist. Knowing that no curative
option exists for MND, she started using Chinese
talismans obtained from a religious practitioner in
China (Fig). She was instructed to burn the Chinese
talismans to ashes and ingest the ashes dissolved in
water 3 times daily. She continued this practice
for about 1 month, until she believed that it was not
useful for her illness. She was then found to have
elevated blood lead level (BLL) of 1.83 µmol/L or
38 µg/dL (reference level, <0.48 µmol/L or <10 µg/dL)
during routine screening for treatable causes of
neuropathy. Her blood mercury level was normal.
Blood lead level rechecked 2 weeks later was 2.61
µmol/L (54 µg/dL). Other than the neurological
symptoms, the patient had no other clinical features
of lead poisoning such as elevated blood pressure,
anaemia with basophilic stippling, or gastro-intestinal
symptoms. She was subsequently referred
to the poison centre for assessment of lead exposure.
Detailed enquiry did not point to any well-known
source of lead exposure. She had been working as a cleansing worker in a food-processing
factory until she became sick. She had never worked
in any mining industry, metal refinery, glass factory,
or battery factory. She did not have a history of
gunshot wound, nor did she have exposure to lead
paint or ceramic craft. Her husband had normal BLL.
Abdominal X-ray did not reveal lead-containing
foreign materials in the gastro-intestinal tract. She
had used several health supplements including
vitamin preparations and ginkgo biloba extract. The
lead levels of these health supplements were found
to be undetectable. Our suspicions were aroused
when the patient reported that the Chinese talismans were supposed
to be written with cinnabar (硃砂), a red mercuric sulfide containing ore. Substitution of
cinnabar with another red mineral, minium (鉛丹, lead tetroxide), when used as Chinese medicine, has
been reported.2 3 Analysis of the Chinese talisman
by inductively coupled plasma mass spectrometry
revealed a very high lead concentration of 17 342 µg/g,
thus confirming the source of lead exposure.
Her BLL was 2.82 µmol/L (59 µg/dL) about
2 months after stopping the use of the Chinese
talismans. Although her neurological presentation
was not typical of lead neurotoxicity,4 there have been
case reports of lead poisoning mimicking MND.5 6
Moreover, an animal study showed that anterior
horn cells were sensitive to lead toxicity.7 Chelation
therapy with succimer (dimercaptosuccinic acid
[DMSA]) was started in view of these possibilities. A
standard course of DMSA 10 mg/kg 3 times daily
for 5 days, followed by 2 times daily for 14 days was
given.8 Her BLL taken at 6 weeks after completion
of DMSA course was 0.7 µmol/L (14 µg/dL). No
improvement of limb weakness was observed in the
patient 8 weeks after completion of DMSA course.
Further courses of DMSA were judged unnecessary.
The patient continued to have medical follow-up for
MND.
Discussion
This case illustrates a rare source of lead exposure
related to the religious practice of consuming burnt Chinese talisman ashes dissolved in water to
cure a disease. The list of common sources of lead
exposure such as occupational, environmental and
recreational ones, can be found in general medicine
and toxicology textbooks.4 Uncommon and exotic
sources reported in the literature usually involve
traditional medicines, cosmetics, and ingestion of
lead-containing foreign bodies (eg bullet, necklace,
fishing sinker).9 10 11
The use of cinnabar has been described
in Daoism alchemy and traditional Chinese
medicine.12 13 Both lead tetroxide and cinnabar
are red in colour with similar appearance, and
substitution of cinnabar with lead tetroxide in
Chinese medicine has been reported.3 The reason for
the substitution is uncertain but it could be due to
mixing up or related to the higher cost of cinnabar.2
The toxicity of lead tetroxide is known since ancient
times in China. Lead poisoning related to the topical
use of lead tetroxide in Chinese medicine for chronic
ulcer has been reported.12
Before the era of molecular genetics, lead
poisoning was believed to be one of the possible
causes of MND.14 15 Nowadays, with the identification
of different genes implicated in MND, it is believed
that genetic causes account for a significant
proportion of the cases.16 Neurological presentation
of mild lead poisoning includes tiredness, headache,
insomnia, memory loss, and lessened interest in
leisure activities. In severe cases, coma, seizures,
and peripheral neuropathy are possible.4 Lead-induced
peripheral neuropathy is typically a pure
motor disorder with features including footdrop and
wristdrop.4 Severe form of lead-induced peripheral
neuropathy has been reported in causing generalised
weakness mimicking MND.5 6 Unlike MND, lead-induced
peripheral neuropathy is associated with
increased body burden of lead, a temporal sequence
between lead exposure and progression of muscle
weakness, clinical stabilisation or remission after
removal from exposure, and systemic involvement
with other features of lead poisoning such as anaemia
and gastro-intestinal disturbance.17
Chelation therapy is usually not indicated
in asymptomatic adults with BLL of <3.36 µmol/L
(70 µg/dL).4 18 Nevertheless, there is no established
action level in the presence of underlying MND. As
lead-induced peripheral neuropathy is a possible
reversible cause in this patient, chelation therapy
was offered despite only a moderate increase in BLL.
The lack of clinical improvement after cessation
of exposure and normalisation of BLL made the
diagnosis of lead-induced peripheral neuropathy
unlikely in this patient.
Conclusion
Ingestion of burnt Chinese talisman is a possible
source of lead exposure. This rare source of lead poisoning should be considered in a specific group
of patients believing in this religious practice.
References
1. Wu YM. Talismans and spells. Available from: http://taiwanpedia.culture.tw/en/content?ID=2073. Accessed 18
Sep 2013.
2. Ban of cinnabar in Chinese medicine use in Taiwan [in
Chinese]. Available from: http://www.twtcm.com.tw/law-content.php?id=9. Accessed 26 Jun 2014.
3. Lead and mercury content of proprietary Chinese medicine
Babao powder [in Chinese]. Available from: http://www.consumers.org.tw/unit412.aspx?id=459. Accessed 11 Dec
2013.
4. Nelson LS, Lewin NA, Howland MA, Hoffman RS,
Goldfrank LR, Flomenbaum NE. Goldfrank’s toxicological
emergencies, 9th ed. New York, NY: McGraw-Hill Medical;
2011: 1266-83.
5. Boothby JA, DeJesus PV, Rowland LP. Reversible forms
of motor neuron disease. Lead “neuritis”. Arch Neurol
1974;31:18-23. CrossRef
6. Rubens O, Logina I, Kravale I, Eglîte M, Donaghy M.
Peripheral neuropathy in chronic occupational inorganic
lead exposure: a clinical and electrophysiological study. J
Neurol Neurosurg Psychiatry 2001;71:200-4. CrossRef
7. Yokoyama K, Araki S, Akabayashi A, Kato T, Sakai T, Sato
H. Alternation of glucose metabolism in the spinal cord
of experimental lead poisoning rats: microdetermination
of glucose utilization rate and distribution volume. Ind
Health 2000;38:221-3. CrossRef
8. Rogan WJ, Dietrich KN, Ware JH, et al. The effect of
chelation therapy with succimer on neuropsychological
development in children exposed to lead. N Engl J Med
2001;344:1421-6. CrossRef
9. Karri SK, Saper RB, Kales SN. Lead encephalopathy due to
traditional medicines. Curr Drug Saf 2008;3:54-9. CrossRef
10. Levin R, Brown MJ, Kashtock ME, et al. Lead exposures in
U.S. children, 2008: implications for prevention. Environ
Health Perspect 2008;116:1285-93. CrossRef
11. St Clair WS, Benjamin J. Lead intoxication from ingestion
of fishing sinkers: a case study and review of the literature.
Clin Pediatr (Phila) 2008;47:66-70. CrossRef
12. Wu ML, Deng JF, Lin KP, Tsai WJ. Lead, mercury, and
arsenic poisoning due to topical use of traditional Chinese
medicines. Am J Med 2013;126:451-4. CrossRef
13. Hsiao CM. Dao of alchemy. Available from: http://taiwanpedia.culture.tw/en/content?ID=2081. Accessed 18
Sep 2013.
14. Lead and motor neurone disease. BMJ 1978;2:308. CrossRef
15. Kamel F, Umbach DM, Munsat TL, Shefner JM, Hu
H, Sandler DP. Lead exposure and amyotrophic lateral
sclerosis. Epidemiology 2002;13:311-9. CrossRef
16. Rademakers R, van Blitterswijk M. Motor neuron disease
in 2012: novel causal genes and disease modifiers. Nat Rev
Neurol 2013;9:63-4. CrossRef
17. Windebank A J, McCall JT, Dyck PJ. Metal neuropathy:
peripheral neuropathy. 3rd ed. Philadelphia: WB Sanders;
1993: 1549-70.
18. Porru S, Alessio L. The use of chelating agents in
occupational lead poisoning. Occup Med (Lond)
1996;46:41-8. CrossRef