Hong Kong Med J 2014 Aug;20(4):304–12 | Epub 6 Jun 2014
DOI: 10.12809/hkmj134168
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Comparison of different intubation techniques
performed inside a moving ambulance: a manikin study
KB Wong, MB, BS1; CT Lui, MB,
BS, FHKAM (Emergency Medicine)1; William YW Chan, BSc
(Hons), MScPEC1,2; TL Lau, MBA, B Bus
(HRM)2; Simon YH Tang, FRCSEd, FHKAM (Emergency
Medicine)1; KL Tsui, FRCSEd, FHKAM (Emergency Medicine)1,2
1 Department of Accident
and Emergency, Tuen Mun Hospital, Tuen Mun, Hong Kong
2 Auxiliary Medical
Service, AMS Headquarters, 81 Princess Margaret Road, Hong Kong
Corresponding author: Dr KL Tsui (tsuikl@ha.org.hk)
Abstract
Objective: Airway
management and endotracheal intubation may be required urgently
when a patient deteriorates in an ambulance or aircraft during
interhospital transfer or in a prehospital setting. The
objectives of this study were: (1) to compare the effectiveness
of conventional intubation by Macintosh laryngoscope in a moving
ambulance versus that in a static ambulance; and (2) to compare
the effectiveness of inverse intubation and GlideScope
laryngoscopy with conventional intubation inside a moving
ambulance.
Design: Comparative
experimental study.
Setting: The experiment
was conducted in an ambulance provided by the Auxiliary Medical
Service in Hong Kong.
Participants: A group of
22 doctors performed endotracheal intubation on manikins with
Macintosh laryngoscope in a static and moving ambulance. In
addition, they performed conventional Macintosh intubation,
inverse intubation with Macintosh laryngoscope, and GlideScope
intubation in a moving ambulance in both normal and simulated
difficult airways.
Main outcome measures: The
primary outcome was the rate of successful intubation. The
secondary outcomes were time taken for intubation, subjective
glottis visualisation grading, and eventful intubation
(oesophageal intubation, intubation time >60 seconds, and
incisor breakage) with different techniques or devices.
Results: In normal
airways, conventional Macintosh intubation in a static ambulance
(95.5%), conventional intubation in a moving ambulance (95.5%), as well as GlideScope intubation in a moving ambulance (95.5%) were
associated with high success rates; the success rate of inverse
intubation was comparatively low (54.5%; P=0.004). In difficult
airways, conventional Macintosh intubation in a static ambulance
(86.4%), conventional intubation in a moving ambulance (90.9%),
and GlideScope intubation in a moving ambulance (100%) were
associated with high success rates; the success rate of inverse
intubation was comparatively lower (40.9%; P=0.034).
Conclusions: En-route
intubation in an ambulance by conventional Macintosh
laryngoscopy is superior to inverse intubation unless the
cephalad access is impossible. GlideScope laryngoscopy appears
to be associated with lower rates of eventful intubation in
difficult airways and has better laryngoscopic view versus
inverse intubation.
New knowledge added by this
study
- The intubation success rates with conventional Macintosh laryngoscopy in static and moving ambulances were high.
- The high failure rate and prolonged time associated with inverse intubation technique made it less useful for en-route intubation unless the cephalad access of the patient was not feasible.
- The study demonstrated high intubation success rate of and slightly longer intubation time with GlideScope intubation in a moving ambulance. GlideScope intubation was associated with lower rates of eventful intubation versus inverse intubation in the setting of difficult airways.
- En-route intubation in an ambulance using conventional Macintosh laryngoscopy at a speed of 20 km/h can be considered a viable option, especially when stopping the transport vehicle is impossible and dangerous.
- The use of video-assisted airway management (GlideScope) could be a backup plan for en-route intubation in the setting of difficult airways, if available.
Introduction
Airway management may be required urgently
when a patient deteriorates in an ambulance during interhospital
transfer or in a prehospital setting. En-route intubation in an
ambulance is challenging due to patient and environmental factors.1 These may include
inadequate or over-exposed lighting, limited access to the
patient, a continuously moving environment, confined space, and
unanticipated patient deterioration. The success rate of en-route
intubation (89.6%) is lower than that of hospital intubation
(98.8%) and intubation-on-scene (94.9%) in air medical transport.2 Intubation success is more
likely in a hospital setting (odds ratio [OR]=8.70) or at the
scene (OR=2.3) compared with en-route intubation.2
Some studies3 4 suggest using inverse
intubation in an entrapped or confined environment. In
inverse intubation, the intubator crouches or kneels near the
patient’s right side, while holding the laryngoscope in the right
hand. Patient’s mouth is opened with the intubator’s left hand.
The laryngoscope blade is gently pulled up and towards the
patient’s feet at a 45° angle. The endotracheal tube is passed
between the visualised vocal cords. The success rate and time of
intubation of using inverse intubation in air transport were not
significantly different from those with conventional intubation in
air transport.5 Inverse
intubation is particularly useful in circumstances where the
cephalad access to the patient is limited. In addition, the
mechanical advantages of pulling up the larynx with the dominant
hand may, theoretically, facilitate visualisation of vocal cords
of patients with difficult airways.
In recent years, portable video
laryngoscope (GlideScope; Verathon Inc, Bothell [WA], US) was
introduced to facilitate airway management in the prehospital
setting.6 7 GlideScope was the first commercially available
video laryngoscope. It uses a high-resolution camera embedded into
a plastic laryngoscope blade, and a LED light for illumination.
The distal angulation makes it ideally suitable for visualising
and intubating over the anterior larynx. The endotracheal tube has
to be used with a special stylet to match the gentle curve of 60°
of the GlideScope blade. It has been proven to be a useful adjunct
for intubation in both normal and difficult airways in selected
settings.8 9 10
The objectives of our experimental study
were: (1) to compare the effectiveness of conventional intubation
by Macintosh laryngoscope in a moving ambulance versus that in a
static ambulance; (2) to compare the effectiveness of inverse
intubation and GlideScope laryngoscopy (model: GVL 4) with
conventional intubation inside a moving ambulance.
Methods
Participants
This was a comparative experimental study
conducted from June to October 2012. Altogether, 22
doctors—including emergency medicine trainees, members, and
fellows—were recruited to participate voluntarily in the study.
All participants were working in the accident and emergency
department (AED) and had been practising emergency medicine for at
least 2 months. All of them had experience in performing
endotracheal intubation in patients. The approval of ethics
committee was considered waived as the study was performed on
manikins and did not involve patients.
Demographic data of the participating
doctors including age, gender, AED working experience, previous
attendance of advanced airway training workshop, past experience
of using inverse intubation and GlideScope on living or dead
patients were collected. Advanced airway training workshop is a
full-day course organised by the Hong Kong College of Emergency Medicine. Course attendants learn
the basic skills of endotracheal intubation. Various airway
adjuncts such as GlideScope are demonstrated and opportunities
provided for participants to practise intubation with these during
the course.
Pre-experiment preparation
The use of conventional Macintosh
laryngoscopy, inverse intubation with Macintosh laryngoscope and
GlideScope laryngoscopy were demonstrated to participants
individually by the experiment conductor using an “AIRSIM” manikin
at least 1 week before the study. The participants were allowed
hands-on practice of the techniques and devices, freely, in a
training room before the experiment.
Experiment setting
The experiment was conducted in an
ambulance provided by the Auxiliary Medical Service. The ambulance
we used was Mercedes-Benz 516CDI measuring approximately 1.6 m in
width and 2.2 m in length. The stretcher, together with the
manikin, was locked on the right side of the ambulance, as in real
life. The intubator would have limited room to kneel down at the
vertex of the patient to perform conventional Macintosh and
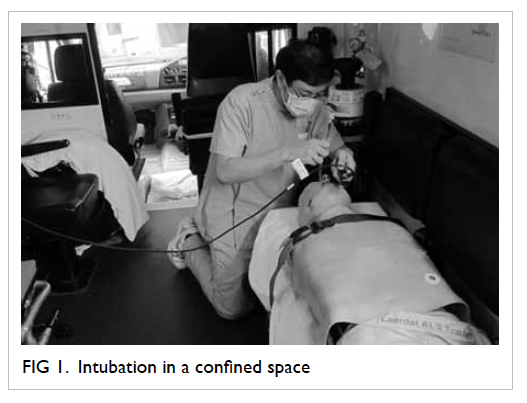
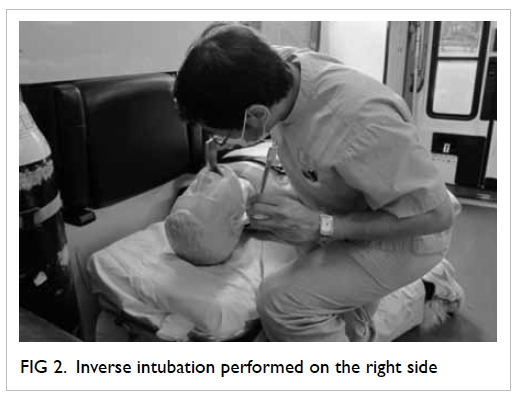
GlideScope intubations (Fig 1). Inverse intubation was performed on
the right side of the manikin (Fig 2). The ambulance was moving at a speed
of 20 km/hour, following a fixed route chosen before the
experiment within the hospital compound. Moving at this relatively
slow speed was only possible on the chosen route as there were a
number of turnarounds and road bumpers.
Intubation setting
The Laerdal “Adult Basic” manikin was used
in the study. A neck collar was applied to the manikin to restrict
the neck mobility and simulate a difficult airway. Size-3 blade
was used for conventional Macintosh and inverse intubations. All
intubations were performed with a 7.5-mm cuffed endotracheal tube.
All participants performed intubations on the manikin in both
normal and difficult airways inside a static ambulance and moving
ambulance. Participants performed the conventional Macintosh,
inverse Macintosh and GlideScope intubations in both normal and
simulated difficult airways inside the moving ambulance in the
same sequence. Neither external manipulation of the larynx nor
airway management adjunct was allowed in the study.
The time required for intubation was
recorded with electronic stopwatch and corrected to one decimal
place. The start time was defined when the participant was asked
to begin while sitting on the couch, approximately 1 metre from the
manikin, with the equipment in hands. The end of the procedure was defined when the participant verbally stated that the
airway was secured with inflation of the cuffed balloon of the
endotracheal tube. The verification of the endotracheal tube
placement was performed by direct visualisation and inflation of
the artificial lung, with no air leakage from the manikin. Both
oesophageal intubation and intubation with time taken longer than
60 seconds were considered to be unsuccessful procedures. Incisor
breakage was reported by the participants when a “click” sound was
heard during intubation; however, it was not considered an
unsuccessful intubation. Participants also reported the
Cormack-Lehane laryngoscopic grading system (C&L grade; grade
1-4) and their preferences for intubation techniques and devices.
Eventful intubation was defined as incisor break, oesophageal
intubation, or intubation taking longer than 60 seconds.
Data analysis
We used SPSS version 16.0 for Windows for
statistical analysis. Rates of successful intubation and incisor
breakage were presented in percentage. The working experience of
participants and time spent on intubation were described by median
and interquartile range as the data showed skewed distribution.
The time required for intubation by different intubation
techniques and devices were analysed by Wilcoxon signed rank test
for paired data. The rates of successful intubation, complications
including oesophageal intubation, incisor breakage and the
subjective visualisation grading system among different intubation
techniques and devices were compared using Fisher’s exact test
with or without Freeman-Halton extension. Spearman’s correlation
was employed to show the relationship between time of intubation
and AED experience. The results were regarded as statistically
significant if P<0.05.
Results
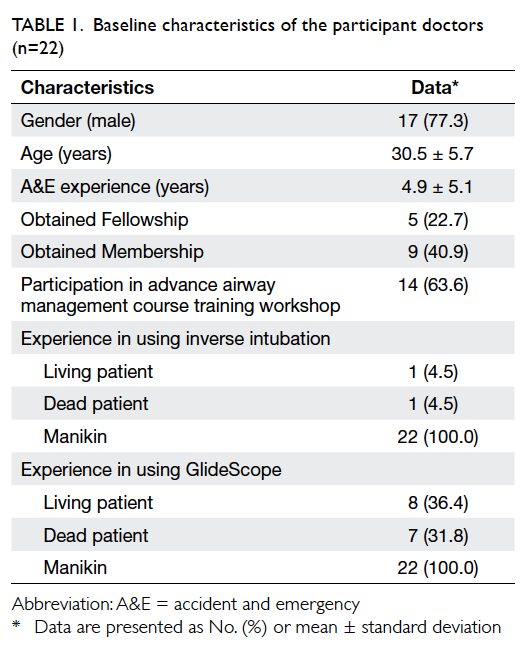
A total of 22 AED (17
male and 5 female) doctors participated in the experiment. The
median age of the participants was 30.5 years. The mean AED working
experience of the participants was 4.9 years. As the technique and
devices were demonstrated by the experiment conductor before
beginning the experiment, all doctors had experience with using
inverse intubation and GlideScope in a manikin. The details are
shown in Table 1. All participants performed
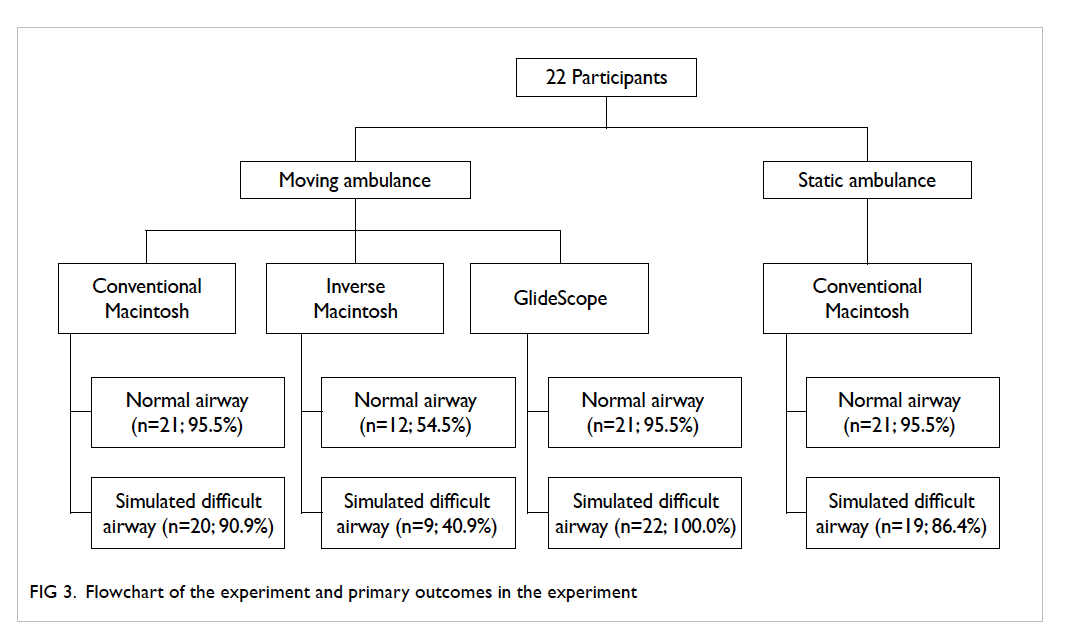
intubations in the eight scenarios and the success rate of each
scenario was summarised in Figure 3.
Conventional intubation in static versus moving
ambulance
The percentage of successful and
unsuccessful intubations, time required for intubation, subjective
glottis visualisation score, and complication rates using
conventional Macintosh intubation in static and moving ambulance
are shown in Table 2. In normal airways, the intubation
success rates in both static (95.5%) and moving ambulances (95.5%)
were high. The median intubation times for intubation in static
and moving ambulances were 21.2 seconds and 26.5 seconds,
respectively (P=0.268). In difficult airways, the intubation
success rates in static and moving ambulances were 86.4% and
90.9%, respectively. The median intubation times in static and
moving ambulances were 22.6 seconds and 20.6 seconds, respectively
(P=0.488). There was no significant difference in the
Cormack-Lehane grades and incidence of eventful intubation between
the two groups.
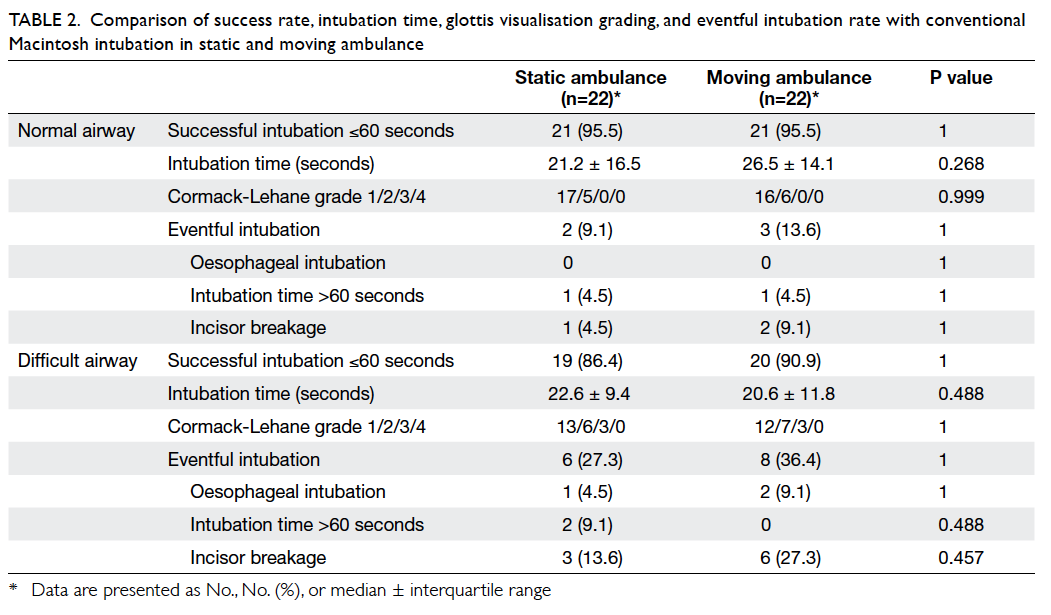
Table 2. Comparison of success rate, intubation time, glottis visualisation grading, and eventful intubation rate with conventional Macintosh intubation in static and moving ambulance
Conventional intubation versus inverse
intubation in a moving ambulance
The intubation performance using the
conventional Macintosh laryngoscopy and inverse Macintosh
intubation in a moving ambulance is shown in Table
3. In normal airways, the success rate of conventional
intubation (95.5%) was significantly higher than that of inverse
intubation (54.5%; P=0.004). The median intubation time with the
conventional technique (26.5 seconds) was shorter than that with
inverse intubation (37.8 seconds; P=0.043). The number of difficult laryngeal visualisation (ie Cormack-Lehane grade ≥3) was
significantly higher with inverse intubation technique (n=8;
36.4%) versus the conventional technique (0%; P<0.001). The
incidence of eventful intubation with inverse intubation (81.8%)
was significantly greater than that with conventional intubation
(13.6%; P<0.001). In difficult airways, the intubation success
rate of conventional technique (90.9%) was also significantly
higher than that of inverse intubation (40.9%; P=0.034). The
median intubation time required for conventional intubation
technique (20.6 seconds) was significantly shorter than that for
inverse intubation (51.3 seconds; P=0.002). The number of
difficult airway intubations was significantly higher with inverse
technique (n=12; 54.5%) than with conventional technique (13.6%;
P=0.003). The incidence of eventful intubation was significantly
higher in the inverse intubation group (81.8%) than that in the
conventional intubation group (36.4%; P=0.002).
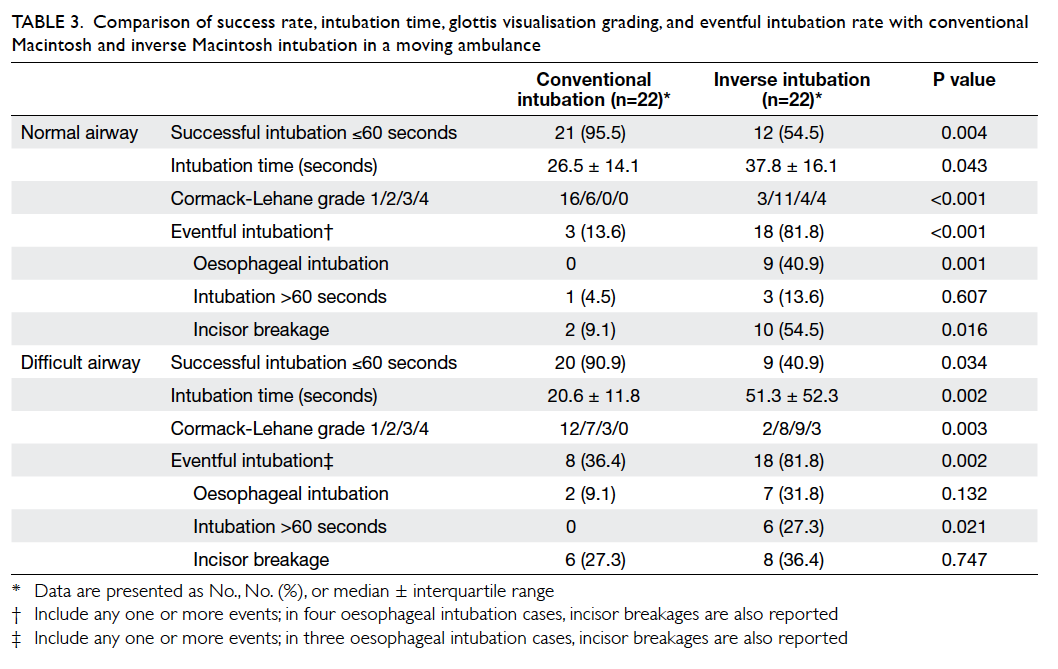
Table 3. Comparison of success rate, intubation time, glottis visualisation grading, and eventful intubation rate with conventional Macintosh and inverse Macintosh intubation in a moving ambulance
Conventional intubation versus GlideScope
intubation in a moving ambulance
The intubation performance using
conventional Macintosh and GlideScope laryngoscopes in a moving
ambulance is summarised in Table 4. In normal airways, the conventional
intubation technique (95.5%) and GlideScope laryngoscopy (95.5%)
were associated with high success rates. The median intubation
time with conventional technique (26.5 seconds) was shorter than
that with GlideScope (31.0 seconds; P=0.012). In difficult
airways, both conventional technique (90.9%) and GlideScope (100%)
were associated with high success rates. The median intubation
time with conventional technique (20.6 seconds) was significantly
shorter than that with GlideScope (32.4 seconds; P<0.001). None
of the intubations with GlideScope in both normal and difficult
airways was given Cormack-Lehane grade of ≥3 but no statistical
difference could be demonstrated in the grades when compared with
conventional intubation in both normal (P=0.721) and difficult
airways (P=0.180). There was an obvious trend for less eventful
intubation with GlideScope (9.1%) versus the conventional
intubation group (36.4%; P=0.069).
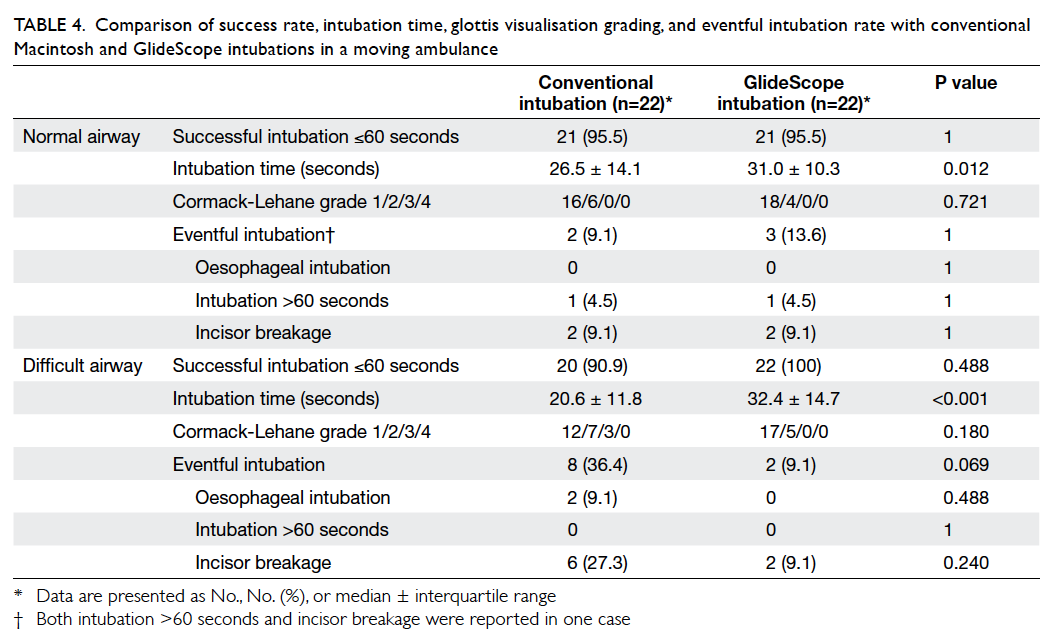
Table 4. Comparison of success rate, intubation time, glottis visualization grading, and eventful intubation rate with conventional Macintosh and GlideScope intubations in a moving ambulance
The relationship between the time required
for intubation and AED experience is presented in Figure
4. An experienced doctor in AED required less time for
conventional intubation in both normal (P=0.043) and difficult
airways (P=0.019) in a static ambulance. Also, experienced doctors
did better with conventional intubation than inverse intubation in
normal airways in a moving ambulance (P=0.019).
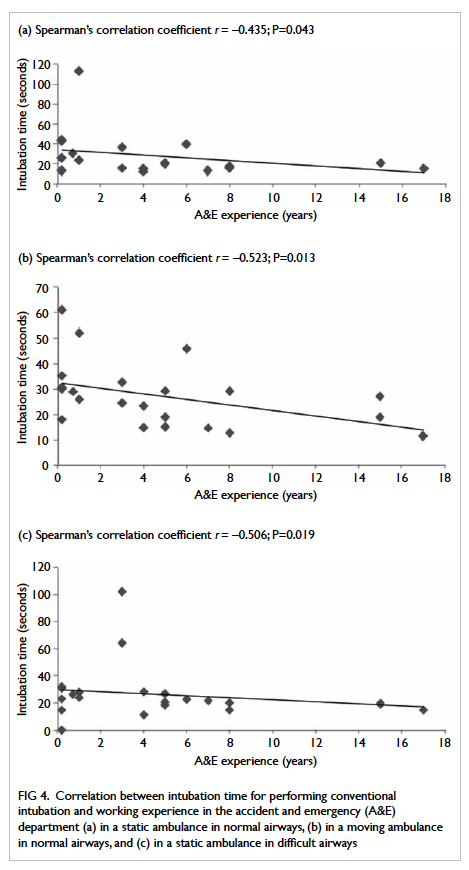
Figure 4. Correlation between intubation time for performing conventional intubation and working experience in the accident and emergency (A&E) department (a) in a static ambulance in normal airways, (b) in a moving ambulance in normal airways, and (c) in a static ambulance in difficult airways
Data on the doctors' perception of the new
technique and device were also collected. Overall, two (9.1%) and
17 (77.3%) doctors thought that inverse intubation and GlideScope
were, respectively, useful as adjuncts in normal airways, while
one (4.5%) and 19 (86.4%) thought that inverse intubation and
GlideScope were, respectively, useful in difficult airways.
Discussion
Previous studies found a 7% to 10%
incidence of difficult intubation in prehospital emergency
en-route intubations.11 12 A number of patient and
environmental factors contribute towards the difficulty in
en-route intubation.1
Environmental factors including restricted space, continuous
movement of the ambulance, and inadequate lighting are believed to
adversely affect the en-route intubation compared with intubation
in a controlled hospital setting. In our study, we found that the
success rates of conventional Macintosh intubation in normal and
difficult airways were high in static and moving ambulances. There
was no significant difference in oesophageal intubation rate,
intubation time, laryngeal visualisation scores, and incisor
breakage rate with conventional Macintosh intubation in static and
moving ambulances. The environment of a moving ambulance did not
appear to hinder the ability of conventional Macintosh intubation
in our experiment. Gough et al13
also recruited 20 emergency medical technicians at the
advanced-intermediate level of EMT (Emergency Medical Technician)
to perform intubation on a manikin in a moving ambulance and
static station. They also found no significant difference in the
success rates and time required for intubation between the two
groups. Stopping an ambulance or a helicopter for en-route
intubation may be impossible or dangerous in real life. Our study
suggests that en-route intubation is feasible in an ambulance
moving at a speed of 20 km/hour.
Inverse intubation has been proposed by
Hilker and Genzwuerker3 as
“an important alternative for intubation in the street”. The
technique was proven to be useful as adjunct in failed
conventional intubation and an important backup position if access
from behind the patient’s head is impossible.4 5 14 In our study, we found that inverse
intubation in an ambulance was associated with higher failure
rate, prolonged intubation, and more complication rates versus
conventional intubation. The clinical usefulness of this technique
in a moving ambulance was not established in our study. Besides,
one of the reported complications of inverse intubation is
pharyngeal laceration.15
If this complication is not recognised, it could result in
significant haemorrhage or potentially lethal infection.
Individual experience is a significant determining factor for the
success of the technique. During the experiment, we also found
that it was quite inconvenient for the intubators who wore
spectacles to perform inverse intubation as the spectacles were
likely to fall off due to the peculiar posture required when
performing the procedure. Inverse intubation would be a reasonable
choice for trained rescuer who cannot position himself/herself to
the space above the victim’s (eg entrapment).
GlideScope has been shown to facilitate
tracheal intubation by improving the laryngeal view in manikin
studies,7 8 9
emergency settings,16 17 18
and a wide spectrum of selective surgeries.19 20 21 Struck et al6 conducted a retrospective observational study
and survey of experiences in prehospital intubation for a 3-year
period. Around 15% of the patients presented with multiple traumas
or failed intubation with conventional laryngoscopy and required
intubation by GlideScope. In our study, we demonstrated high
intubation success and low failure rates with GlideScope
laryngoscopy, but the median time for intubation was slightly
longer versus that with the conventional Macintosh laryngoscopy in
normal airways (P=0.012) and difficult airways (P<0.001). The
finding of longer intubation time with GlideScope was also
demonstrated in previous studies.16
19 20 However, some studies found no difference in
the intubation time.7 22 One study8 even found that GlideScope enables
faster intubation in patients with cervical spine immobilisation. The wide range of results
may be attributed to the differences in experience with using
GlideScope, different study settings (manikin vs real patient), and
different study scenarios (normal vs difficult airway). Piepho et
al23 conducted a study
among paramedics who used the Macintosh and GlideScope video
laryngoscopes for intubating manikins. They found that the
intubation time with GlideScope was longer than that with
Macintosh in the first and second attempts of intubation. However,
no significant difference in time required for intubation was
observed in the subsequent attempts. This confirms a rapid
learning curve for intubation with GlideScope. In another manikin
study with 60 anaesthetists, GlideScope was found to have a steep
learning curve for intubation but, after five attempts,
differences in terms of time of endotracheal intubation persisted
when compared with the Macintosh laryngoscopy.24 In our study, there was a trend for less eventful intubation with GlideScope (P=0.069) in the setting of difficult airways. Thus, we recommend its use as a backup for en-route
intubation, especially in difficult airway settings. In real-life
practice of using GlideScope, the passage of endotracheal tube
through the deeply curved and rigid stylet may be hindered. An
assistant is required to thread the endotracheal tube into the
trachea while the intubator holds the GlideScope in position. This
is expected to be more difficult in an ambulance because of
limited space.
This study had several limitations.
Firstly, we used a manikin in our study rather than a real
patient; thus, the results may not be transferrable to real
patients. However, we believe that the use of new techniques and
devices in airway management is not ethical in clinically unstable
and emergency patients. A well-designed manikin-based study would
be an acceptable choice for the aforementioned reasons. Secondly,
only one of the difficult airway situations was tested in our
study. Other difficult airway situations in daily practice such as
limited mouth opening, tongue oedema, and presence of blood/vomitus were not studied. Thirdly, there was the issue of learning
curve associated with new techniques and devices. Overall, one
(4.5%) and eight (36.4%) of the participants had previous
experience of using inverse intubation and GlideScope in clinical
settings, respectively. Although we demonstrated the use of
inverse intubation and GlideScope and allowed participants to
practise freely at least 1 week before the experiment, we cannot
demonstrate the non-inferior result associated with the use of
inverse intubation in a previous study.5
We also observed that the intubation time for difficult airways in
a moving ambulance was shorter than that for normal airways. The
most likely explanation is the learning effect and intubation
experience. The participants performed different intubation
techniques in normal airways followed by the same techniques in
difficult airways in a moving ambulance. The participants may have
gained experience from working in a continuously moving
environment. We suggest further studies with inverse intubation
and GlideScope after a longer period of training and practice to
examine for the reproducibility of these results. Fourthly, the
study was performed inside our hospital which has imposed speed
limits on vehicles moving on the road. Moving at a relatively slow
speed of 20 km/hour was only possible in the chosen route as
there were a number of turnarounds and road bumpers. Moreover, we
limited the speed in order to avoid any danger to or fall of
participants. Fifthly, GlideScope (model: GVL 4) for the
experiment was chosen because it was the only model available in
our hospital. Other models that are specifically designed for
prehospital use such as Glidescope Ranger may be a better choice,
if available. Lastly, the sample size of the study was relatively
small and could have inadequate power to detect real differences
between some comparison, for example, comparison of the eventful
intubation rate between GlideScope and conventional intubation.
Conclusions
Our study demonstrates an overall high
intubation success rate with conventional Macintosh and GlideScope
laryngoscopes in a moving ambulance. The time required for
intubation with GlideScope was longer than that with conventional
laryngoscope. Application of GlideScope should be suggested as an
adjunct for intubation in an ambulance in the presence of
adequately trained staff. The high failure rate and prolonged time
associated with the inverse intubation technique make it less
useful than conventional intubation and GlideScope intubation
unless the cranial access of the patient is restricted.
Acknowledgements
We would like to thank the Auxiliary
Medical Service, the Hong Kong SAR Government for providing the
ambulance and all physicians who participated in this experimental
study.
References
1. Helm M, Hossfeld B, Schäfer,
Hoitz J, Lampl L. Factors influencing emergency intubation in the
pre-hospital setting—a multicentre study in the German Helicopter
Emergency Medical Service. Br J Anaesth 2006;96:67-71. CrossRef
2. McIntosh SE, Swanson ER, McKeone
A, Barton ED. Location of airway management in air medical
transport. Prehosp Emerg Care 2008;12:438-42. CrossRef
3. Hilker T, Genzwuerker HV.
Inverse intubation: an important alternative for intubation in the
streets. Prehosp Emerg Care 1999;3:74-6. CrossRef
4. Hoyle JD Jr, Jones JS, Deibel M,
Lock DT, Reischman D. Comparative study of airway management
techniques with restricted access to patient airway. Prehosp Emerg
Care 2007;11:330-6. CrossRef
5. Robinson K, Donaghy K, Katz R.
Inverse intubation in air medical transport. Air Med J
2004;23:40-3. CrossRef
6. Struck MF, Wittrock M, Nowak A.
Prehospital Glidescope video laryngoscopy for difficult airway
management in a helicopter rescue program with anaesthetists. Eur
J Emerg Med 2011;18:282-4. CrossRef
7. Nakstad AR, Sandberg M. The
GlideScope Ranger video laryngoscope can be useful in airway
management of entrapped patients. Acta Anaesthesiol Scand
2009;53:1257-61. CrossRef
8. Lim TJ, Lim Y, Liu EH.
Evaluation of ease of intubation with the GlideScope or Macintosh
laryngoscope by anaesthetists in simulated easy and difficult
laryngoscopy. Anaesthesia 2005;60:180-3. CrossRef
9. Benjamin FJ, Boon D, French RA.
An evaluation of the GlideScope, a new video laryngoscope for
difficult airways: a manikin study. Eur J Anaesthesiol
2006;23:517-21. CrossRef
10. Cooper RM, Pacey JA, Bishop
MJ, McCluskey SA. Early clinical experience with a new
videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth
2005;52:191-8. CrossRef
11. Adnet F, Jouriles NJ, Le
Toumelin P, et al. Survey of out-of-hospital emergency intubations
in the French prehospital medical system: a multicenter study. Ann
Emerg Med 1998;32:454-60. CrossRef
12. Combes X, Jabre P, Jbeili C,
at al. Prehospital standardization of medical airway management:
incidence and risk factors of difficult airway. Acad Emerg Med
2006;13:828-34. CrossRef
13. Gough JE, Thomas SH, Brown LH,
Reese JE, Stone CK. Does the ambulance environment adversely
affect the ability to perform oral endotracheal intubation?
Prehosp Disaster Med 1996;11:141-3.
14. Koetter KP, Hilker T,
Genzwuerker HV, et al. A randomized comparison of rescuer
positions for intubation on the ground. Prehosp Emerg Care
1997;1:96-9. CrossRef
15. Smally AJ, Dufel S, Beckham J,
Cortes V. Inverse intubation: potential for complications. J
Trauma 2002;52:1005-7. CrossRef
16. Platts-Mills TF, Campagne D,
Chinnock B, Snowden B, Glickman LT, Hendey GW. A comparison of
GlideScope video laryngoscope versus direct laryngoscopy
intubation in the emergency department. Acad Emerg Med
2009;16:866-71. CrossRef
17. Mosier JM, Stolz U, Chiu S,
Sakles JC. Difficult airway management in the emergency
department: GlideScope videolaryngoscopy compared to direct
laryngoscopy. J Emerg Med 2012;42:629-34. CrossRef
18. Sakles JC, Mosier JM, Chiu S,
Keim SM. Tracheal intubation in the emergency department: a
comparison of GlideScope® video laryngoscopy to direct
laryngoscopy in 822 intubations. J Emerg Med 2012;42:400-5. CrossRef
19. Kim JT, Na HS, Bae JY, et al.
GlideScope video laryngoscope: a randomized clinical trial in 203
paediatric patients. Br J Anaesth 2008;101:531-4. CrossRef
20. Andersen LH, Rovsing L, Olsen
KS. GlideScope videolaryngoscope vs. Macintosh direct laryngoscope
for intubation of morbidly obese patients: a randomized trial.
Acta Anaesthesiol Scand 2011;55:1090-7. CrossRef
21. Griesdale DE, Liu D, McKinney
J, Choi PT. Glidescope® video-laryngoscopy versus direct
laryngoscopy for endotracheal intubation: a systematic review and
meta-analysis. Can J Anaesth 2012;59:41-52. CrossRef
22. Teoh WH, Sexena S, Shah MK,
Sia AT. Comparison of three videolaryngoscopes: Pentax Airway
Scope, C-MAC, Glidescope vs the Macintosh laryngoscope for
tracheal intubation. Anaesthesia 2010;65:1126-32. CrossRef
23. Piepho T, Weinert K, Heid FM,
Werner C, Noppens RR. Comparison of the McGrath® Series 5 and
GlideScope® Ranger with the Macintosh laryngoscope by paramedics.
Scand J Trauma Resusc Emerg Med 2011;19:4. CrossRef
24. Savoldelli GL, Schiffer E,
Abegg C, Baeriswyl V, Clergue F, Waeber JL. Learning curves of the
Glidescope, the McGrath and the Airtraq laryngoscopes: a manikin
study. Eur J Anaesthesiol 2009;26:554-8. CrossRef