Hong
Kong Med J 2014 Aug;20(4):274–8 | Epub
28 Feb 2014
DOI: 10.12809/hkmj134062
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
The association between clinical parameters and
glaucoma-specific quality of life in Chinese primary open-angle
glaucoma patients
Jacky WY Lee, FRCS1; Catherine WS Chan, MPhil1;
Jonathan CH Chan, FRCS2; Q Li, PhD1; Jimmy
SM Lai, MD1
1 Department of
Ophthalmology, The University of Hong Kong, Pokfulam,
Hong Kong
2 Department of
Ophthalmology, Queen Mary Hospital, Pokfulam, Hong
Kong
Corresponding author: Dr Jacky WY Lee (jackywylee@gmail.com)
Abstract
Objective: To
investigate the association between
clinical measurements and glaucoma-specific quality
of life in Chinese glaucoma patients.
Design: Cross-sectional
study.
Setting: An academic
hospital in Hong Kong.
Patients: A Chinese
translation of the Glaucoma
Quality of Life–15 questionnaire was completed
by 51 consecutive patients with bilateral primary
open-angle glaucoma. The binocular means of
several clinical measurements were correlated with
Glaucoma Quality of Life–15 findings using Pearson’s
correlation coefficient and linear regression. The
measurements were the visual field index and
pattern standard deviation from the Humphrey
Field Analyzer, Snellen best-corrected visual acuity,
presenting intra-ocular pressure, current intra-ocular
pressure, average retinal nerve fibre layer thickness
via optical coherence tomography, and the number
of topical anti-glaucoma medications being used.
Results: In these
patients, there was a significant
correlation and linear relationship between a poorer
Glaucoma Quality of Life–15 score and a lower
visual field index (r=0.3, r2=0.1,
P=0.01) and visual
acuity (r=0.3, r2=0.1, P=0.03). A
thinner retinal
nerve fibre layer also correlated with a poorer Glaucoma Quality
of Life–15 score, but did not
attain statistical significance (r=0.3, P=0.07). There
were no statistically significant correlations for the
other clinical parameters with the Glaucoma Quality
of Life–15 scores (all P values being >0.7). The three
most problematic activities affecting quality of life
were “adjusting to bright lights”, “going from a light
to a dark room or vice versa”, and “seeing at night”.
Conclusion: For Chinese
primary open-angle
glaucoma patients, binocular visual field index and
visual acuity correlated linearly with glaucoma-specific
quality of life, and activities involving dark
adaptation were the most problematic.
New knowledge added by this
study
- A lower visual field index and poorer visual acuity correlated with a poorer glaucoma-specific quality of life in Chinese primary open-angle glaucoma patients.
- The most problematic activities affecting quality of life in glaucoma patients were “adjusting to bright lights”, “going from a light to a dark room or vice versa”, and “seeing at night”.
- In busy clinical settings, the visual field index serves as a quick reference for glaucoma-specific quality of life, and can identify patients who may warrant more formal assessment for psychosocial support.
- Lifestyle modifications for glaucoma patients can include more light in dark areas and adjusting curtains and mirrors to reduce glare, so as to make the transition from different lighting conditions more acceptable.
Introduction
In clinical practice, much time is spent on
measuring
the clinical parameters of glaucoma including the
intra-ocular pressure (IOP), visual acuity (VA), visual
field, and retinal nerve fibre layer (RNFL) thickness.
What is often neglected is the quality of life (QOL)
of patients and how well they live with their disease
on a day-to-day basis. Glaucoma affects 80 million people
worldwide.1 It is a chronic
and irreversible
disease with a heavy burden on visual function and
vision, besides being one of the most important
constituents affecting QOL.2
3 4
Recourse to QOL questionnaires in glaucoma
can be broadly divided into general health–related,
vision-specific, or glaucoma-specific.5
Quality-of-life
assessment in glaucoma patients is as important as the clinical
parameters used to measure glaucoma
progression, because it reflects the impact of
the ocular disease on the patient as a whole and
may also be an indicator of whether the disease is
advancing.4 6
7 8
9
Using generic QOL assessments, glaucoma
was found to have deleterious impact as other
systemic chronic diseases like osteoporosis, diabetes,
or dementia.10 However,
such generic tests do not
address the end points of glaucoma, such as visual
impairment and visual field constriction, for which
reason their robustness and specificity are limited.10
There are approximately 18 different patient-reported
QOL assessments specific to glaucoma.
Among these, the Glaucoma Quality of Life–15
Questionnaire (GQL-15) and the Vision and Quality
of Life Index have been found most satisfactory in
terms of content, validity, and reliability.11
Thus, the
aim of this study was to investigate the correlations
between clinical parameters and glaucoma-specific
QOL in Chinese patients with bilateral primary open-angle glaucoma
(POAG).
Methods
For this cross-sectional study, consecutive
patients with bilateral POAG were recruited from an academic
hospital in Hong Kong. The diagnosis of POAG was
based on an open angle on gonioscopy, a presenting
IOP of >21 mm Hg, and either a glaucomatous visual
field loss on at least two Humphrey visual field tracings
using the 24-2 SITA fast protocol (Humphrey
Instruments, Inc, Zeiss Humphrey, San Leandro
[CA], US) or RNFL thinning on Spectralis Optical
Coherence Tomography (Heidelberg Engineering,
Carlsbad [CA], US). Patients were excluded if they
had unilateral disease, concomitant ocular diseases
that significantly affected their vision (amblyopia,
mature cataract affecting the accuracy of glaucoma
investigations). Patients were also excluded if they
had other corneal or retinal pathologies, or if they
were unable to yield reliable visual field results. Their
IOPs were determined using Goldmann applanation
tonometry.
The GQL-15 questionnaire is
glaucoma-specific,
and assesses patient-perceived visual
disability in 15 daily tasks responded to in writing.
The tasks addressed four aspects of visual disability:
(1) central and near vision; (2) peripheral vision; (3)
dark adaptation and glare; and (4) outdoor mobility.
A 5-point rating scale for the level of difficulty of each
task can yield a total score of 0 to 75. Higher scores
signify a lower QOL. The GQL-15 was translated
into traditional Chinese text and distributed to
participating patients. For illiterate patients, the
items were read out to them in Cantonese dialect.
The questionnaire was translated from English to
Chinese by an investigator who was fluent in both
English and Chinese. The translated questionnaire
was checked for discrepancies by a second
investigator and a consensus was reached to develop
a draft Chinese questionnaire. A third investigator
then back-translated the draft Chinese questionnaire
into English; the back-translated draft and the
original version were then compared. Discrepancies
were amended and gave rise to the final Chinese
version. The questionnaire was then tested on five
POAG patients of varying gender and age. Patients
were asked to complete the questionnaire, and offer
their own interpretation of its contents and whether
any alternative wording should be used.
The D’Agostino-Pearson omnibus test was
used
to test for normality. Nearly half of the parameters
passed the normality testing. The means of several
clinical parameters were calculated for the two eyes
and correlated with the GQL-15 using Pearson’s
correlation coefficient and linear regression analysis.
The selected parameters were the visual field index
(VFI) and pattern standard deviation (PSD) from the
Humphrey Field Analyzer, the Snellen best-corrected
VA, the presenting IOP, current IOP, average RNFL
thickness via optical coherence tomography, as well
as the number of topical anti-glaucoma medications
being used. t Tests were used to test for differences
between the mean GQL-15 scores between males
and females. Data were expressed as mean ± standard
deviation (SD). Any P value of <0.05 was accepted as
statistically significant.
Our institutional review board granted
ethics
approval for the study and informed consent was
obtained from each patient prior to the start of the
study.
Results
Fifty-one patients with bilateral POAG were
recruited, all of whom were Chinese. Their mean
(± SD) age was 65.8 ± 12.1 years and the male-to-female
ratio was 1.1:1.
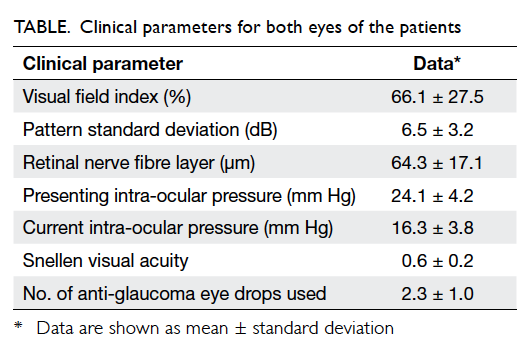
The means of their clinical parameters for
both
eyes are shown in the Table.
Their mean GQL-15
score was 26.0 ± 11.6 (out of 75). The three most
problematic activities reported for all patients
belonged to: item 4 “adjusting to bright lights” (mean
score, 2.3 ± 1.3); item 6 “going from a light to a dark
room or vice versa” (mean score, 2.3 ± 1.3); and item
2 “seeing at night” (mean score, 2.2 ± 1.2).
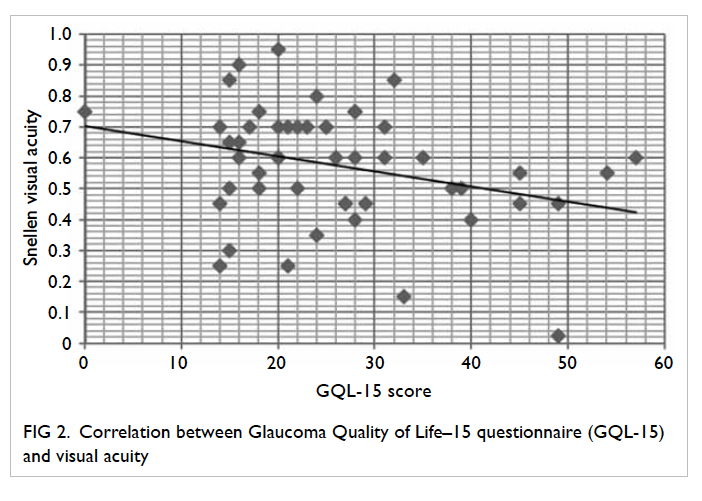
There was a moderately significant
correlation
between a lower VFI and a poorer GQL-15 score
(r=0.3, P=0.01; Fig
1). Likewise, a poorer VA
correlated significantly with a poorer GQL-15 score
(r=0.3, P=0.03; Fig
2). These two correlations seemed
to follow a linear pattern such that linear regression
analysis showed a weak linear relationship between
a poorer GQL-15 score and a lower VFI (r2=0.1,
P=0.01) and a poorer VA (r2=0.1, P=0.03).
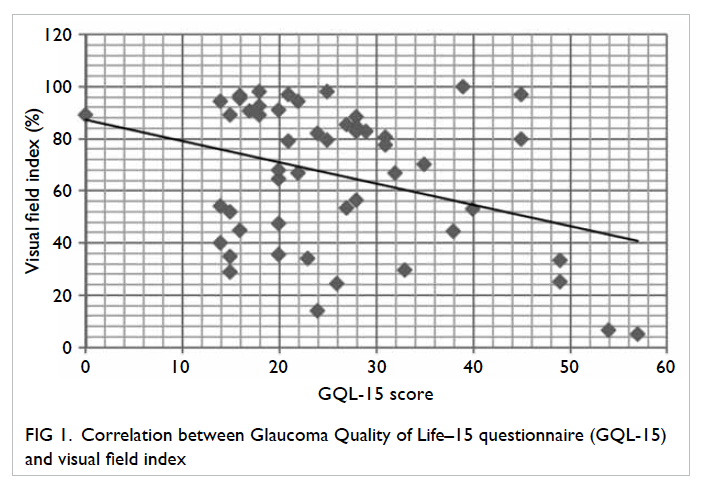
Fig 1. Correlation between Glaucoma Quality of Life–15 questionnaire (GQL-15) and visual field index
A thinner RNFL appeared to be associated
with
a poorer GQL-15 score but the correlation did not
attain statistical significance (r=0.3, P=0.07). In terms
of pressure control, a higher presenting IOP showed
a trend towards correlation with a poorer GQL-15
score (r=0.2) as did a lower current IOP (r= 0.2)
and
a greater number of anti-glaucoma eye drops used
(r=0.1). However, none of these correlations reached
statistical significance (all P>0.7). On comparing
GQL-15 scores between male and female glaucoma
patients, no significant difference was found (P=0.3,
t test).
Discussion
Various studies have associated QOL with
visual field
impairment.8 12
Odberg et al13 simply
categorised
visual field defects into “normal”, “having a restricted
scotoma”, or “having a field defect large enough to be
of visual significance”, and found a weak-to-moderate
correlation between such visual field defects and
subjective visual disabilities. The Collaborative
Initial Glaucoma Treatment Study later found
that at the time of diagnosis, patients’ visual fields
correlated only modestly with a health-related QOL
questionnaire and that of VFIs; mean
deviation (MD) showed better correlation with QOL
than PSD, corrected pattern SD,
or short-term fluctuation.14
Nelson et al4 found
that the GQL-15 scores, and especially the subsets
pertaining to glare, correlated significantly with MD,
even for patients with mild disease. Furthermore,
those with moderate and severe visual field loss had similar
GQL-15 scores, suggesting a threshold
for disability may be reached up to a certain level of
glaucoma severity4 or
represent adaptation to loss
of visual function. Similarly, Goldberg et al15
have
found that the GQL-15 scores correlated with VA,
MD, the number of binocular points of <10 dB, and
that QOL tended to decrease with disease severity.
Whilst MD is commonly correlated with QOL in
glaucoma patients, it has the drawback of not being
specific enough to represent the limitations caused
by glaucoma alone, since it may also be affected by
global defects like cataract. On the other hand, using
PSD eliminates the factor of global defects, though
it is not sensitive in advanced glaucoma, where the
entire field is globally depressed.
Thus in this study, we utilised the VFI,
which
is a percentage summarising the overall visual field
status compared to age-adjusted visual fields. The
VFI emphasises the importance of the central field.
It is less affected by media opacities (cataracts), and
is more accurate than MD for monitoring glaucoma
progression.16 17
Few studies have used VFI to correlate
with QOL in glaucoma. Sawada et al18
reported that
VFI correlated with QOL via the 25-item National
Eye Institute Visual Function Questionnaire (NEI
VFQ-25) and that the correlation was better than
with MD. Our study found a statistically significant
correlation between the reduction in mean binocular
VFI and a poorer GQL-15 score and that VFI was
a better indicator of glaucoma-specific QOL than
RNFL thickness, IOP, or PSD on visual field. We chose
to use PSD rather than MD in our analysis because
the latter could be affected by any global obstruction
to vision like cataract, whereas PSD is more specific
for inter-field variability. However, the two clinical
parameters that achieved a significant correlation
with the GQL-15 score were binocular VFI and VA,
and both parameters were also associated with the
GQL-15 score in a linear manner.
Intra-ocular pressure control did not
correlate
significantly with QOL although a higher IOP on
presentation seemed to produce a lower QOL score,
and interestingly a lower current IOP seemed to
correlate with a poorer QOL. This unique finding may
indicate that those with a lower current IOP have had
glaucoma for longer or have more advanced disease
warranting more aggressive pressure reduction.
Furthermore, those using more anti-glaucoma eye
drops seemed to have a lower QOL score, but these
correlations were weak and did not reach statistical
significance.
Patient perceptions of disease and methods
of coping are heavily influenced by culture and
ethnicity. Thus, Singapore Chinese glaucoma patients
were more accepting of their daily disabilities than
corresponding American Caucasians.19
Literature
pertaining to Chinese glaucoma patients is sparse.
Wu et al20 found that
Chinese glaucoma patients were particularly concerned about the
uncertainties
of treatment, the prognosis, and passing on of the
disease to family members. Lin and Yang21
reported
a correlation with MD and the Medical Outcomes
Study Short-Form 36 Health Survey and the NEI
VFQ-25. Whilst clinical data provide evidence
of structural and functional damage of the optic
nerve, they do not address the impact of disease
on patients. The correlation of objective clinical
measurements to QOL is particularly useful, because
it gives ophthalmologists in a busy clinical setting an
overall impression of glaucoma-specific QOL. This
can enable them to recommend environmental and
lifestyle modifications to minimise obstacles and
maximise the period of independence.5
Our study
found that in Chinese glaucoma patients, the most
problematic aspects of coping were “adjusting to
bright lights”, “going from a light to a dark room
or vice versa”, and “seeing at night”. Interestingly,
all these activities belong to the realm of dark
adaptation. Hence, environmental modifications can
potentially help to reduce glare.4
Furthermore, an
estimation of QOL from clinical parameters can allow
ophthalmologists to more readily identify patients
with a poorer QOL needing more psychosocial
support. Interestingly, it has been reported that
POAG itself is associated with anxiety, depression,
and hypochrondriasis22 and
a low GQL-15 score has
also been identified as a predictor for depression.23
One limitation of our study was that it was
cross-sectional and looked at POAG patients with
varying degrees of severity. A longitudinal study
would have provided additional information about
the changes in QOL throughout different stages
of the disease. A second limitation was that the
population received heterogeneous treatments
(lasers and surgeries). However, as the aim of this
study did not involve evaluating the side-effects of
glaucoma treatments and since the GQL-15 too
did not target treatment side-effects, we did not
consider it necessary to exclude those who had
undergone such treatments previously. Rather,
we opted to include a more heterogeneous POAG
population to make the results more generalisable
and representative. A third limitation was that no
single test is perfect; the GQL-15 mainly focuses on
visual activities, which is only one aspect of QOL.
Conceivably, such a questionnaire only reflects
patient confidence to perform certain tasks rather
than the actual difficulties experienced. Nevertheless,
it has been shown that patients’ loss of confidence
often precedes their perceptions of difficulty.24
To the best of our knowledge, this is one
of the
few studies reporting a significant correlation and a
linear relationship between VFI and the glaucoma-specific
GQL-15 score in the Chinese POAG
patients. This study also identified dark adaptation
as the most challenging visual issue pertinent to Chinese POAG
patients.
Declaration
No conflicts of interest were declared by
the authors.
References
1. Mansberger SL, Demirel S. Early
detection of glaucomatous visual field loss: why, what, where, and
how. Ophthalmol Clin North Am 2005;18:365-73, v-vi. CrossRef
2. Beauchamp CL, Beauchamp GR,
Stager DR Sr, Brown MM, Brown GC, Felius J. The cost utility of
strabismus surgery in adults. J AAPOS 2006;10:394-9. CrossRef
3. Brown GC, Brown MM, Sharma S, et
al. The burden of age-related macular degeneration: a value-based
medicine analysis. Trans Am Ophthalmol Soc 2005;103:173-86.
4. Nelson P, Aspinall P,
Papasouliotis O, Worton B, O’Brien C. Quality of life in glaucoma
and its relationship with visual function. J Glaucoma
2003;12:139-50. CrossRef
5. Spaeth G, Walt J, Keener J.
Evaluation of quality of life for patients with glaucoma. Am J
Ophthalmol 2006;141(1 Suppl):S3-14. CrossRef
6. Jampel HD, Schwartz A, Pollack
I, Abrams D, Weiss H, Miller R. Glaucoma patients' assessment of
their visual function and quality of life. J Glaucoma
2002;11:154-63. CrossRef
7. Janz NK, Wren PA, Lichter PR,
Musch DC, Gillespie BW, Guire KE. Quality of life in newly
diagnosed glaucoma patients: the Collaborative Initial Glaucoma
Treatment Study. Ophthalmology 2002;108:887-97; discussion 898. CrossRef
8. Parrish RK 2nd, Gedde SJ, Scott
IU, et al. Visual function and quality of life among patients with
glaucoma. Arch Ophthalmol 1997;115:1447-55. CrossRef
9. Gutierrez P, Wilson MR, Johnson
C, et al. Influence of glaucomatous visual field loss on
health-related quality of life. Arch Ophthalmol 1997;115:777-84. CrossRef
10. Mills T, Law SK, Walt J,
Buchholz P, Hansen J. Quality of life in glaucoma and three other
chronic diseases: a systematic literature review. Drugs Aging
2009;26:933-50. CrossRef
11. Vandenbroeck S, De Geest S,
Zeyen T, Stalmans I, Dobbels F. Patient-reported outcomes (PRO's)
in glaucoma: a systematic review. Eye (Lond) 2011;25:555-77. CrossRef
12. Lee BL, Gutierrez P, Gordon M,
et al. The Glaucoma Symptom Scale. A brief index of
glaucoma-specific symptoms. Arch Ophthalmol 1998;16:861-6. CrossRef
13. Odberg T, Jakobsen JE,
Hultgren SJ, Halseide R. The impact of glaucoma on the quality of
life of patients in Norway. II. Patient response correlated to
objective data. Acta Ophthalmol Scand 2001;79:121-4. CrossRef
14. Mills RP, Janz NK, Wren PA,
Guire KE. Correlation of visual field with quality-of-life
measures at diagnosis in the Collaborative Initial Glaucoma
Treatment Study (CIGTS). J Glaucoma 2001;10:192-8. CrossRef
15. Goldberg I, Clement CI, Chiang
TH, et al. Assessing quality of life in patients with glaucoma
using the Glaucoma Quality of Life–15 (GQL-15) questionnaire. J
Glaucoma 2009;18:6-12. CrossRef
16. Bengtsson B, Heijl A. A visual
field index for calculation of glaucoma rate of progression. Am J
Ophthalmol 2008;145:343-53. CrossRef
17. Casas-Llera P, Rebolleda G,
Muñoz-Negrete FJ, Arnalich-Montiel F, Pérez-López M,
Fernández-Buenaga R. Visual field index rate and event-based
glaucoma progression analysis: comparison in a glaucoma
population. Br J Ophthalmol 2009;93:1576-9. CrossRef
18. Sawada H, Fukuchi T, Abe H.
Evaluation of the relationship between quality of vision and the
visual function index in Japanese glaucoma patients. Graefes Arch
Clin Exp Ophthalmol 2011;249:1721-7. CrossRef
19. Saw SM, Gazzard G, Au Eong KG,
Oen F, Seah S. Utility values in Singapore Chinese adults with
primary open-angle and primary angle-closure glaucoma. J Glaucoma
2005;14:455-62. CrossRef
20. Wu PX, Guo WY, Xia HO, Lu HJ,
Xi SX. Patients' experience of living with glaucoma: a
phenomenological study. J Adv Nurs 2011;67:800-10. CrossRef
21. Lin JC, Yang MC. Correlation
of visual function with health-related quality of life in glaucoma
patients. J Eval Clin Pract 2010;16:134-40. CrossRef
22. Erb C, Thiel HJ, Flammer J.
The psychology of the glaucoma patient. Curr Opin Ophthalmol
1998;9:65-70. CrossRef
23. Skalicky S, Goldberg I.
Depression and quality of life in patients with glaucoma: a
cross-sectional analysis using the Geriatric Depression Scale–15,
assessment of function related to vision, and the Glaucoma Quality
of Life–15. J Glaucoma 2008;17:546-51. CrossRef
24. Nelson P, Aspinall P, O’Brien
C. Patients’ perception of visual impairment in glaucoma: a pilot
study. Br J Ophthalmol 1999;83:546-52. CrossRef