Hong Kong Med J 2014;20:229–33 | Number 3, June 2014 | Epub 28 Mar 2014
DOI: 10.12809/hkmj134064
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Current management practice for bladder cancer
in Hong Kong: a hospital-based cross-sectional survey
Eddie SY Chan, MD, FHKAM (Surgery); CH
Yee, FRCS (Edin), FHKAM (Surgery);
SM Hou,FRCS (Edin), FHKAM (Surgery);
CF Ng, MD, FHKAM (Surgery)
Division of Urology, Department of Surgery,
Prince of Wales Hospital, The
Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr Eddie SY Chan (eddie@surgery.cuhk.edu.hk)
Abstract
Objectives: To examine
current practice in the
management of bladder cancer in Hong Kong
government and private hospitals.
Design: Cross-sectional
survey.
Setting: All government
hospitals and the major
private institutions in Hong Kong, which provide
urological services.
Participants: Urologists
responding to an
anonymous, self-administered, web-based
questionnaire regarding practices in smoking
cessation, treatment of non-muscle invasive bladder
cancer and muscle invasive bladder cancer, and
research into bladder cancer.
Results: Of the 29
urologists from 11 government
hospitals and eight private institutions who were
invited, 18 from 11 (100%) government hospitals
and seven from six (75%) private institutions
responded, which amounted to an 86% response
rate. In all, 88% of the respondents seldom or never
referred their bladder cancer patients to smoking
cessation programmes. Hong Kong urologists
showed good compliance in the management of
non-muscle invasive bladder cancer according to
international guidelines. There was great variation
with regard to regimens for maintenance of intravesical
immunotherapy. There was underuse
of perioperative systemic chemotherapy, despite
wide acceptance of this practice; fewer than 10%
of the patients received neo-adjuvant and adjuvant
systemic chemotherapy for the treatment of muscle
invasive bladder cancer. Of the surveyed urologists,
80% expressed an inadequacy of resources for
bladder cancer research and 96% agreed that a local
inter-hospital bladder cancer database was needed.
Conclusions: This study
demonstrated great
diversity in the use of intravesical immunotherapy,
perioperative systemic chemotherapy, and surgical
treatment of bladder cancer among urology service
providers. There is a need for clear recommendations
in these areas.
New knowledge added by this
study
- By providing important information on practice preferences in the management of bladder cancer in both the public and private sectors in Hong Kong, this study demonstrates the great diversity in the use of intravesical immunotherapy, perioperative systemic chemotherapy, and surgical treatments.
- Local guidelines in bladder cancer management and the use of intravesical bacillus Calmette-Guérin are needed.
Introduction
Bladder cancer is a common genitourinary
malignancy. It is the fifth most frequent cancer
in the US, where it accounts for 7% of all incident
malignancies.1 In 2009, there were 372 newly
diagnosed bladder cancer cases in Hong Kong.2
Patients with bladder cancer warrant close
surveillance because of high recurrence and
progression rates (50-70%).3 Due to its prolonged
natural history, intensive follow-up and treatment
strategies, management of this cancer is costly and is the most
expensive malignancy to treat on a per-patient
basis.4 5
Guidelines for bladder cancer management
have been established in an attempt to improve
treatment outcomes. The most commonly used
are the American Urological Association (AUA),
European Association of Urology (EAU), and
National Comprehensive Cancer Network (NCCN)
guidelines. There is no specific guideline in Hong
Kong. The practice in bladder cancer treatment
in Hong Kong may differ among urologists and centres. The aim of
this survey was to gain
better understanding of current bladder cancer
management practice in Hong Kong.
Methods
Questionnaire and data collection
An online multiple-choice questionnaire was
sent
to all government hospitals and major private
institutions providing urological services. Senior
urologists from corresponding hospitals were
invited to respond to the questionnaire, which was
anonymous, self-administrated, and non-validated.
From each centre at least one urologist was
encouraged to respond. If the hospital or centre had
three or more board-certified urologists, no more
than two were encouraged to complete the survey, so
as to be as representative as possible. The responses
from the surveyed urologists were submitted and
collected over a secured connection.
The questionnaire comprised 30 questions
divided into three sections: (1) General Issues
and Smoking Cessation, (2) Management and
Treatment, and (3) Bladder Cancer Research. The
first part concerned the daily workload for bladder
cancer and smoking cessation programmes. The
second part (the main part of the survey) evaluated
management preferences for non-muscle invasive bladder cancers
(NMIBCs) and muscle invasive
bladder cancers (MIBCs), and included questions
regarding intravesical and systemic chemotherapy.
The final part addressed the adequacy of resources
and progress for bladder cancer research.
Statistical analysis
Data were presented as descriptive
statistics of the
main variables and analysed using Excel (Version 14.2,
California, US). A frequency table was constructed
to indicate the management preferences.
Results
Between March and August 2012, 19 hospitals
and
institutions from both government (n=11) and
private (n=8) sectors were involved in this study.
Twenty-nine senior urologists from corresponding
hospitals were invited to participate in the survey.
Responses from 11 (100%) government hospitals and
six (75%) private sector institutions were received.
Of the 29 invited urologists, 18 were from public
hospitals and 11 from private institutions; eventually,
25 (86%) responded to the survey and completed the
questionnaires (18 [100%] from public hospitals and
7 [64%] from the private sector).
Part 1: general issues and smoking cessation
Among the surveyed urologists, 17 (68%)
estimated
that 10% to 25% of their clinical workload was spent
on diagnosis, treatment, and surveillance of bladder
cancer. Whilst cigarette smoking is a key risk factor
for bladder cancer, 14 (56%) commented that there
was no access to a smoking cessation programme in
their hospitals. Notably, 22 (88%) seldom or never
referred their patients to any smoking cessation
programme. Only 11 (44%) and 10 (40%) of the
respondents thought that resources for smoking
cessation were readily or easily available to patients
and urologists, respectively.
Part 2: management and treatment
Guidelines from AUA and EAU remain the most
useful guides for bladder cancer management.
None of the surveyed urologists used the guideline
published by the Chinese Urological Association.
However, 12 (48%) of the respondents had a bladder
cancer management guideline in their own hospital
and 15 (60%) expressed the need for a local Hong
Kong guideline.
Among the surveyed hospitals, immediate
intravesical chemotherapy was always (56%) or
often (44%) administered. All hospitals (100%)
used mitomycin C as the chemotherapeutic drug
of choice. Currently, international guidelines also
advocate a second transurethral resection of the
bladder tumour (TURBT) for patients with high-risk
NMIBC or in the absence of detrusor muscle in bladder tissue
specimens. While all the respondents
from government hospitals adopted this concept,
five (28%) of them “always”, and 13 (72%) of them
“often” performed a second TURBT. On the contrary,
four (57%) of the urologists in private institutions
seldom practised a second procedure. Overall, the
common problems of a second TURBT encountered
by urologists included a tight operation schedule
(48%) and refusal by patients (16%).
All the surveyed hospitals always (44%) or
often
(56%) prescribed intravesical bacillus Calmette-Guérin (BCG) for
high-risk NMIBC patients.
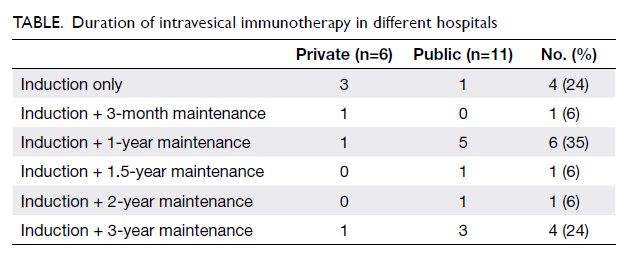
However, there was a great variation in the duration
of intravesical immunotherapy regimens in the 17
hospitals with responding urologists. The Table
shows that the durations ranged from induction with
no maintenance (24%), to maintenance for 3 months
(6%), 1 year (35%), 1.5 years (6%), 2 years (6%),
and 3 years (24%). Of the 25 surveyed urologists,
76% (n=19) encountered problems in intravesical
immunotherapy, which were related to the poor
patient compliance stemming from side-effects
(60%) and serious BCG-related complications (16%).
Open radical cystectomy remains the most
common approach in Hong Kong. Of the 17 surveyed
hospitals whose urologists responded, only three
(18%) government hospitals routinely practised
radical cystectomy with a minimally invasive
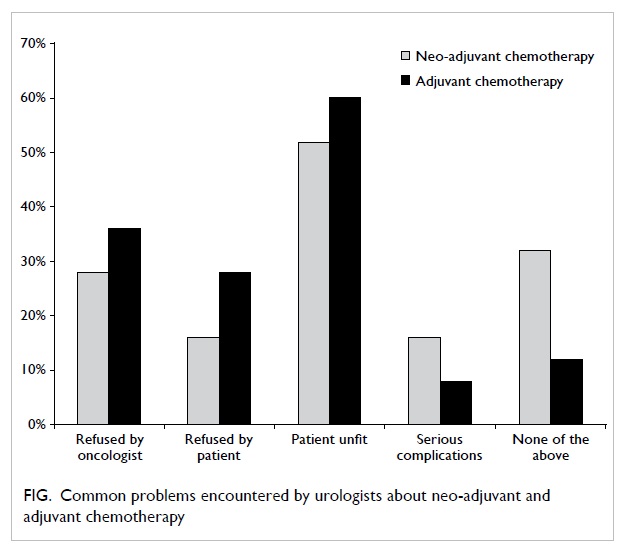
approach. Most of the surveyed urologists thought
that systemic chemotherapy was useful in selected
MIBC patients in neo-adjuvant (56%) and adjuvant
(76%) settings. However, all but one hospital reported
that less than 10% of their patients received either
neo-adjuvant or adjuvant chemotherapy. The low
frequency of systemic perioperative chemotherapy
could be due to patient refusal or poor tolerance
of systemic chemotherapy. Oncologists’ refusal to
provide chemotherapy in neo-adjuvant (28%) and
adjuvant (36%) settings could also be the reason
(Fig).
Part 3: bladder cancer research
Among the respondents, 13 (52%) thought
that
current management regimens were adequate
for diagnosing and preventing bladder cancer
recurrence/progression, whilst 12 (48%) felt that
progress on bladder cancer treatment research was
poor compared to that for renal cell and prostate
cancer. Most of the respondents (80%) stated
that resources for bladder cancer research were
inadequate, and most (96%) also expressed a need
for an inter-hospital bladder cancer database to
improve patient care.
Discussion
Bladder cancer is among the commonest
urological
malignancies. Patients with bladder cancer demand
close surveillance for recurrence and progression.
Thus, one fourth of the workload of
urologists is
spent on the diagnosis, treatment, and surveillance
of bladder cancer patients. Because of the
complicated treatment and follow-up strategies, it is
also the most costly to treat,4 5 and there is a wide
variation in the practice patterns and compliance to
guidelines.6 In Hong Kong, bladder cancer incidence
is on a decreasing trend in both sexes, but the crude
mortality rate has not changed in the last decade.2
There are no data available regarding the preferred
management patterns of Hong Kong urologists on
bladder cancer. Herein, we report on the first cross-sectional
survey of clinical practice for a specific
urological disease category in Hong Kong. Such
information can be important for urologists, health
policy-makers, and patients.
Smoking is the most important preventable
cause of death in Hong Kong and many countries.
Diseases caused by smoking impose a heavy economic and medical
burden on our society.
Many countries therefore have enhanced efforts
to promote smoking cessation in addition to
strengthening tobacco control measures and
legislation. Cigarette smoking is a well-established
risk factor for bladder cancer, and accounts for up
to 50% of all incident bladder cancers.7 The risk of
bladder cancer in smokers is 2 to 5 times higher than
that in non-smokers. Smoking cessation decreases
the bladder cancer risk as well as the recurrence
rate of such tumours.8 Continuing to smoke is
associated with worse cancer-related outcomes
than in those who quit. In this context, urologists
play a vital role in influencing patient knowledge
about smoking risks and encouraging cessation of
the habit. Guzzo et al9 reported that 76% of bladder
cancer patients in tertiary referral centres received
no specific intervention to aid smoking cessation.
A number of trials confirmed that interventions
from trained health care professionals increase
success rates in smoking cessation attempts.10
At present, there are a number of local smoking
cessation clinics run by the Department of Health
(Tung Wah Group of Hospitals, the Pok Oi Hospital,
the Hospital Authority, and other organisations).
These programmes cover a comprehensive range of
activities that include smoking cessation services,
education for the public, and research. In our study,
88% of the respondents seldom or never referred
their patients to any smoking cessation programme,
and nearly 60% claimed that smoking cessation
facilities were difficult for patients and doctors to
access. This is a disappointing statistic that needs to
be addressed.
International guidelines set forth by the
AUA,
EAU, and NCCN are widely adopted by Hong Kong
urologists. There is good consensus on the practice
of second TURBT and perioperative intravesical
chemotherapy between different guidelines for
NMIBC patients.11 Evidence supports the use of
single-dose, immediate postoperative intravesical
instillation of mitomycin C to decrease tumour
recurrence. Second TURBT within 6 weeks of
initial resection enables better tissue sampling and
reduces early tumour recurrence. A US study of
14 677 bladder cancer patients between 1997 and
2004 found that only 49 (0.33%) received immediate
intravesical chemotherapy after TURBT.12 Cookson
et al13 reported that 66% of the US-based urologists
never used postoperative intravesical chemotherapy.
Gontero et al14 evaluated the adherence to EAU
guidelines in eight Italian referral centres and found
that only 49% of high-risk patients underwent a repeat
TURBT. A study based on SEER-Medicare data
reported that only 7.7% of patients with high-grade
NMIBC underwent a second TURBT.15 Hong Kong
urologists appear to have excellent compliance with
both intravesical chemotherapy and performance of a second TURBT
in the management of NMIBC
patients. Urologists in the private sector seem to
achieve a lower rate of second TURBT, which may be
due to patient preference, expectations, and financial
concerns.
Intravesical instillation of BCG is a
standard
therapy after TURBT for intermediate or high-risk
NMIBC, as there is evidence that bladder tumour
recurrence or progression is prevented by such
therapy.3 For optimal efficacy, an induction course
followed by maintenance therapy is recommended,
but the duration of maintenance therapy remains
controversial. Böhle et al16 suggested that at least 1
year of maintenance BCG was required to prevent
recurrence or progression. However, a meta-analysis
of 20 trials was unable to determine which BCG
maintenance schedule was the most effective.17
Recently, the benefit of maintenance BCG has been
challenged.18 This practice is further complicated by
significant toxicity and a high treatment cessation
rate. Given the uncertainty surrounding the optimal
intravesical immunotherapy, urologists in Hong
Kong vary in how they deliver such treatment.
Having a consensus on optimal intravesical BCG
therapy is challenging but necessary, before further
research involving randomised clinical trials is
undertaken.
Minimally invasive (laparoscopic/robotic)
surgical approaches have been widely used by
local urologists, including for nephrectomy and
prostatectomy. These help reduce morbidity, shorten
hospital stays, and enhance recovery. Open radical
cystectomy remains the standard treatment for
MIBC patients. Laparoscopic or robot-assisted
radical cystectomy is among the most challenging
procedures and performed in a limited number
of centres where the necessary experience and
expertise exists.19 The situation in Hong Kong is
similar, while open radical cystectomy is the most
preferred approach.
The pattern of treatment for MIBC has
changed
to a multidisciplinary approach. There is growing
evidence that perioperative chemotherapy provides
survival benefits in such patients. Meta-analysis
suggests that neo-adjuvant and probably adjuvant
systemic chemotherapy too increase cancer-specific
and overall survivals.20 21 Porter et al22 reported that
only 2.6% of stage 2 and 12.7% of stage 4 patients
with bladder cancer received either neo-adjuvant
or adjuvant chemotherapy. The underutilisation of
perioperative systemic therapy was also observed in
our survey. Non-tumour–related factors (including
patient age, co-morbidity, and oncologists’
preferences) influence treatment patterns. Such
practice is not consistent with current evidence and
recommendations, all of which may affect outcomes
of bladder cancer patients.
While substantial progress has ensued in
the field of other genitourinary malignancies, bladder
cancer research lags behind. Under-enrolment, lack
of specific funding for bladder cancer, and lack of
cooperative group trials are some of the problems
that research needs to overcome. An inter-hospital
cancer database could provide important information
to clinicians and health care administrators so as to
formulate health care plans. Relevant outcome data
could benefit both urologists and patients, when it
comes to improving bladder cancer treatment.23
There are several limitations to be noted
regarding this study. First, the survey was a
retrospective review of practice. Second, the
reported numbers and percentages were estimations
without any verification, which may have introduced
inaccuracy and recall bias. Third, this was a hospital-based
survey instead of being individual-based,
with 11 government and eight private hospitals that
provide urology services. It nevertheless covered
common local practice in most of the hospitals and
institutions, and should be representative. Fourth,
currently there are about 100 board-certified
practising urologists in Hong Kong, so surveying
a larger number of urologists might have yielded a
broader view of practice patterns at an individual
level.
Conclusions
This study provided important information
on
practice preferences in the management of bladder
cancer in both public hospitals and private institutions
in Hong Kong. It demonstrated great diversity in the
use of intravesical immunotherapy, perioperative
systemic chemotherapy, and surgical treatment of
bladder cancer in different urology centres. There is a
need for clear local recommendations and guidelines
in these areas.
References
1. Jemal A, Siegel R, Xu J, Ward E.
Cancer statistics, 2010. CA Cancer J Clin 2010;60:277-300. CrossRef
2. Hong Kong Cancer Registry,
Hospital Authority. Available from:
http://www3.ha.org.hk/cancereg/. Accessed 4 Nov 2012.
3. Lamm DL, Blumenstein BA,
Crissman JD, et al. Maintenance bacillus Calmette-Guerin
immunotherapy for recurrent TA, T1 and carcinoma in situ
transitional cell carcinoma of the bladder: a randomized Southwest
Oncology Group Study. J Urol 2000;163:1124-9. CrossRef
4. Botteman MF, Pashos CL, Redaelli
A, Laskin B, Hauser R. The health economics of bladder cancer: a
comprehensive review of the published literature.
Pharmacoeconomics 2003;21:1315-30. CrossRef
5. Avritscher EB, Cooksley CD,
Grossman HB, et al. Clinical model of lifetime cost of treating
bladder cancer and associated complications. Urology
2006;68:549-53. CrossRef
6. Chamie K, Saigal CS, Lai J, et
al. Compliance with guidelines for patients with bladder cancer.
Cancer 2011;117:5392-401. CrossRef
7. Zeegers MP, Tan FE, Dorant E,
van Den Brandt PA. The impact of characteristics of cigarette
smoking on urinary tract cancer risk: a meta-analysis of
epidemiologic studies. Cancer 2000;89:630-9. CrossRef
8. Fleshner N, Garland J, Moadel A,
et al. Influence of smoking status on the disease-related outcomes
of patients with tobacco-associated superficial transitional cell
carcinoma of the bladder. Cancer 1999;86:2337-45. CrossRef
9. Guzzo TJ, Hockenberry MS,
Mucksavage P, Bivalacqua TJ, Schoenberg MP. Smoking knowledge
assessment and cessation trends in patients with bladder cancer
presenting to a tertiary referral center. Urology 2012;79:166-71. CrossRef
10. Carson KV, Verbiest ME, Crone
MR, et al. Training health professionals in smoking cessation.
Cochrane Database Syst Rev 2012;(5):CD000214.
11. Brausi M, Witjes JA, Lamm D,
et al. A review of current guidelines and best practice
recommendations for the management of nonmuscle invasive bladder
cancer by the International Bladder Cancer Group. J Urol
2011;186:2158-67. CrossRef
12. Madeb R, Golijanin D, Noyes K,
et al. Treatment of nonmuscle invading bladder cancer: do
physicians in the United States practice evidence based medicine?
The use and economic implications of intravesical chemotherapy
after transurethral resection of bladder tumors. Cancer
2009;115:2660-70. CrossRef
13. Cookson MS, Chang SS, Oefelein
MG, Gallagher JR, Schwartz B, Heap K. National practice patterns
for immediate postoperative instillation of chemotherapy in
nonmuscle invasive bladder cancer. J Urol 2012;187:1571-6. CrossRef
14. Gontero P, Oderda M, Altieri
V, et al. Are referral centers for non-muscle-invasive bladder
cancer compliant to EAU guidelines? A report from the vesical
antiblastic therapy Italian study. Urol Int 2011;86:19-24. CrossRef
15. Skolarus TA, Ye Z, Montgomery
JS, et al. Use of restaging bladder tumor resection for bladder
cancer among medicare beneficiaries. Urology 2011;78:1345-9. CrossRef
16. Böhle A, Jocham D, Bock PR.
Intravesical bacillus Calmette-Guerin versus mitomycin C for
superficial bladder cancer: a formal meta-analysis of comparative
studies on recurrence and toxicity. J Urol 2003;169:90-5. CrossRef
17. Sylvester RJ, van der Meijden
AP, Lamm DL. Intravesical bacillus Calmette-Guerin reduces the
risk of progression in patients with superficial bladder cancer: a
meta-analysis of the published results of randomized clinical
trials. J Urol 2002;168:1964-70. CrossRef
18. Herr HW. Is maintenance
bacillus Calmette-Guérin really necessary? Eur Urol 2008;54:971-3. CrossRef
19. Imkamp F, Herrmann TR,
Rassweiler J, et al. Laparoscopy in German urology: changing
acceptance among urologists. Eur Urol 2009;56:1074-81. CrossRef
20. Stadler WM, Lerner SP.
Perioperative chemotherapy in locally advanced bladder cancer.
Lancet 2003;361:1922-3. CrossRef
21. Advanced Bladder Cancer (ABC)
Meta-analysis Collaboration. Neoadjuvant chemotherapy in invasive
bladder cancer: update of a systematic review and meta-analysis of
individual patient data advanced bladder cancer (ABC)
meta-analysis collaboration. Eur Urol 2005;48:202-5. CrossRef
22. Porter MP, Kerrigan MC, Donato
BM, Ramsey SD. Patterns of use of systemic chemotherapy for
Medicare beneficiaries with urothelial bladder cancer. Urology
2011;29:252-8.
23. Chan ES, Chu SK, Lam KM, Ng
CF. Radical cystectomy for the treatment of bladder cancer: What
have we learnt from Surgical Outcomes Monitoring and Improvement
Program reports? Surg Pract 2012;16:164-7. CrossRef