Hong Kong Med J 2014;20:213–21 | Number 3, June 2014 | Epub 9 May 2014
DOI: 10.12809/hkmj134181
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Social obstetrics: non-local expectant mothers
admitted through accident and emergency department in a public
hospital in Hong Kong
WK Yung, MB, BS, FHKAM (Obstetrics and
Gynaecology)1; Winnie Hui, MB, BS1; YT
Chan, MB, BS, MRCOG1; TK Lo, FHKAM (Obstetrics and
Gynaecology)1; SM Tai, BSc, MSc1; C Sing,
BSc, MSc1; YY Lam, MB, BS, FHKAM (Paediatrics)2;
CM Lo, FRCP (Irel), FHKAM (Emergency Medicine)3; WL Lau,
MB, BS, FRCOG1; WC Leung, MD, FHKAM (Obstetrics and
Gynaecology)1
1 Department of Obstetrics
and Gynaecology, Kwong Wah Hospital, 25 Waterloo Road, Hong Kong
2 Department of
Paediatrics, Kwong Wah Hospital, 25 Waterloo Road, Hong Kong
3 Department of Accident
and Emergency, Kwong Wah Hospital, 25 Waterloo Road, Hong Kong
Corresponding author: Dr WC Leung (leungwc@ha.org.hk)
Abstract
Objectives: To review
the pregnancy outcomes of non-booked, non-local pregnant women
delivering in Kwong Wah Hospital via admission to the Accident
and Emergency Department 1 year after the announcement by the
Hospital Authority to stop antenatal booking for non-eligible
persons; and to perform a literature review of local studies
about non-eligible person deliveries over the last decade.
Design: Case series.
Setting: A public
hospital in Hong Kong.
Participants: All women
who held the People’s Republic of China passport or the two-way
permit and those non-eligible persons whose spouses were Hong
Kong Identity Card holders, who delivered in Kwong Wah Hospital
from 1 April 2011 to 31 March 2012.
Results: Overall, 219
women who were non-eligible persons delivered 221 live births
during the study period. Compared with the annual statistics of
Kwong Wah Hospital in 2011, non-local mothers were of higher
parity; more likely to have hypertensive disease (including
pre-eclamptic toxaemia), preterm deliveries (ie at <37
weeks), babies needing admission to the special care baby unit,
and macrosomic babies (ie weighing >4.0 kg). The rates of
induction of labour and caesarean section were lower in this
group. There was no significant difference in the maternal and
neonatal outcomes between women who had no booking and those who
had a booking in another Hospital Authority or private hospital.
There were many incidents of near-miss obstetric complications
or suboptimally managed obstetric conditions due to lack of
well-structured and continuous antenatal care in this group of
non-eligible persons.
Conclusion: Non-eligible
person delivering babies in Hong Kong has become a social
obstetrics phenomenon. Despite the introduction of policies,
reduction in the number of deliveries (quantity) did not improve
the obstetric outcomes (quality). Health care professionals
should continue to be prepared for managing the potential
near-miss clinical complications in this group of ‘travelling
mothers’.
New knowledge added by this
study
- Non-eligible person (NEP) delivery in Hong Kong has been a social obstetric phenomenon specific to this region (Hong Kong SAR) because of political circumstances. Despite the reduction in the quantity, these non-booked deliveries continue to run a high risk of adverse obstetric outcomes due to difficulties experienced by the expectant mothers in accessing a well-structured obstetric service.
- Regardless of the number of patient load, the NEP women remain potentially at risk of obstetric complications. Health care professionals should be prepared for managing the near-miss conditions.
Introduction
The influx of expectant mothers from
Mainland China leading to overwhelming of the local obstetric and
neonatal services has been a hot topic of discussion in the media
in the past few years. In 2001, the Hong Kong Court of Final
Appeal delivered a unanimous opinion by which Chong Fung-yuen, a
Chinese baby born while his Mainland Chinese parents were in Hong
Kong on two-way permits, was granted residency in Hong Kong. In
addition, in 2003, the Hong Kong SAR Government introduced the
Individual Visit Scheme which allowed travellers from Mainland
China to visit Hong Kong and Macao on an individual basis. Since
the introduction of these policies, there has been a dramatic
increase in the number of ‘traveller’ mothers delivering in Hong
Kong. This ‘birth tourism’—a travel to a country that practises
birthright citizenship or permanent residency in order to give
birth there, so that the child will be a citizen of the
destination country—has significantly influenced the standard
obstetric practice in Hong Kong, resulting in adverse pregnancy
outcomes. We have described this phenomenon as social obstetrics.1 2
3
According to the Hospital Authority (HA)
pay code, there are seven categories of non-eligible person (NEP).
The categories of NE-2 (People’s Republic of China passport or two-way permit holder ‘雙非’) and NE-3 (NEP whose spouse is a Hong Kong Identity Card [HKID] holder ‘單非’) contribute to the majority
of NEP deliveries in public hospitals.
In 2005, the HA launched an obstetric
package to limit the number of non-local women delivering in
public hospitals. The charge was HK$20 000 for 3 days and 2 nights
of hospital stay including delivery. However, this policy did not
discourage ‘traveller’ mothers from delivering in public
hospitals.4
In February 2007, the HA launched a new
obstetric package for non-local expecting mothers. This package
charged almost double (HK$39 000) for the hospitalisation for 3
days and 2 nights. Those who have not booked were additionally
charged.
Unfortunately, the growing number of NEP
deliveries in HA hospitals outweighed the capacity of public
obstetric and neonatal services. In 2010, there were about 88 000
deliveries in the territory, of which 50% were by mainland mothers
(Fig 1a). The total capacity of neonatal
intensive care units (NICUs; about 100 beds) in Hong Kong can only
support an annual delivery rate of 75 000.5 This resulted in the formation of Hong Kong
Obstetric Service Concern Group in March 2011—to urge the Hong
Kong SAR Government to take action in preventing the collapse of
public obstetric and neonatal services. The first remedial measure
was to stop accepting new antenatal booking in HA hospitals from 8
April 2011 till the end of the year. One year later, on 26 April
2012, HA announced that there was no booking quota for non-local
expecting mothers as public service was prioritised for the Hong
Kong citizens to meet the surge of childbirth in the Chinese year
of ‘Dragon’. The non-booked deliveries would be charged HK$90 000
for the 3-days-2-nights package. Lastly, the Government prohibited
antenatal booking of non-local mothers in either public (for NE-2
and NE-3 categories) or private (for NE-2 category) sectors from 1
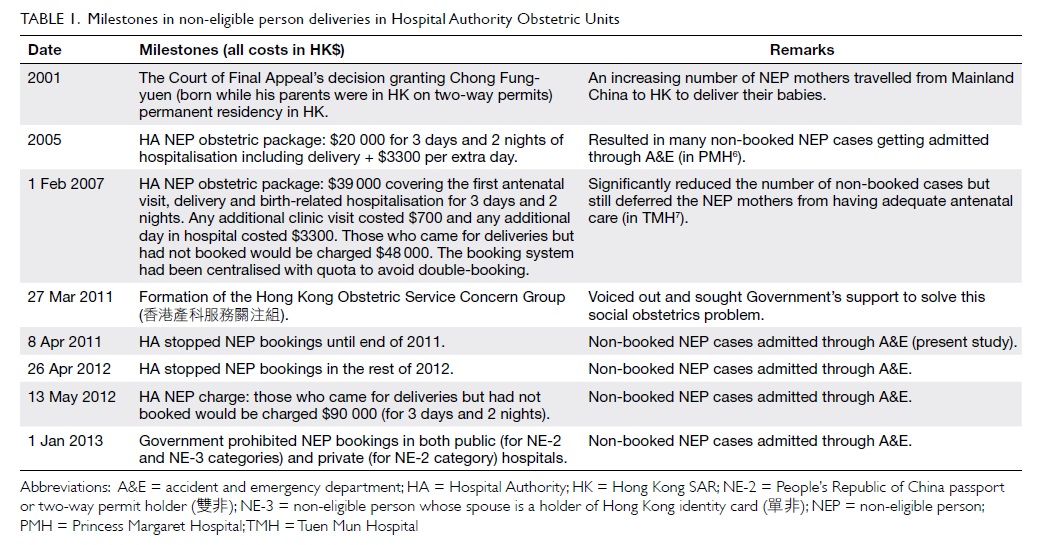
January 2013 onwards (Table 16
7).
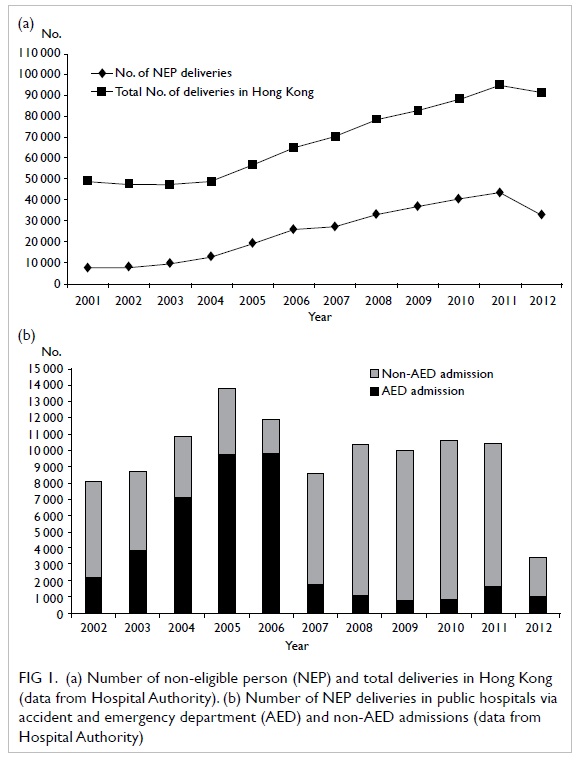
Figure 1. (a) Number of non-eligible person (NEP) and total deliveries in Hong Kong (data from Hospital Authority). (b) Number of NEP deliveries in public hospitals via accident and emergency department (AED) and non-AED admissions (data from Hospital Authority)
However, if a pregnant woman, regardless of
her identity card status, attended the accident and emergency
department (AED) of a public hospital, the doctor-on-duty would
assess her condition and offer admission to the obstetric unit if
medically indicated. The admission rate via AED through the years
varied with the implementation of obstetric package and government
policy (Fig 1b). In 2005, when the first obstetric
package was launched, the admission through AED for delivery was
high. The second package in 2007 encouraged antenatal booking,
and, thus, the AED admission rate dropped thereafter. Since April
2011, HA stopped all antenatal bookings for NEP, as a result of
which the total number of NEP deliveries decreased drastically;
however, the proportion of AED admissions increased.
In Kwong Wah Hospital, antenatal booking
for non-local mothers had been stopped since April 2011. The NEP
deliveries in our unit were mainly through AED admission or
transfer from another HA or private hospital.
This retrospective study reviewed the
pregnancy conditions and outcomes of a cohort of non-booked,
non-local women admitted via AED of Kwong Wah Hospital over a
1-year period.
Methods
This study evaluated the demographics,
peripartum events, and pregnancy outcomes of the non-local
pregnant women (NE-2 and NE-3 categories) who were admitted
through AED and who delivered in Kwong Wah Hospital from 1 April
2011 to 31 March 2012. This was the 1-year period after HA’s
announcement (on 8 April 2011) of stopping antenatal booking for
non-local women. The birth registry record of Kwong Wah Hospital
was reviewed. Women who delivered in the captioned period with no
HKID number were identified. Clinical records of the subjects were
retrieved from the central record unit. Only women in NE-2 and
NE-3 categories were recruited.
Clinical notes and electronic patient
records of the subjects were reviewed. The pregnancy conditions
studied included the presenting symptoms, antenatal complications,
gestation at delivery, mode of delivery, intrapartum and
postpartum complications, birth weight of babies, Apgar score,
need for neonatal resuscitation, admission to NICU or special baby
care unit, neonatal morbidities, congenital abnormalities, etc.
Maternal and neonatal outcomes were further analysed according to
their booking status before admission. The annual statistics of
Kwong Wah Hospital 2011 were used as reference.
Statistical analysis
Skewed continuous variables and nearly
normally distributed variables were presented as medians
(interquartile ranges) and means (± standard deviations [SDs]),
respectively. Categorical data were presented as counts and
percentages. Mann-Whitney U test and independent sample t
test were used for comparison of medians and means, respectively.
Pearson Chi squared test or Fisher’s exact test were used for
comparisons of frequencies, where appropriate. All analyses were
performed with the Statistical Package for the Social Sciences
(Windows version 16.0; SPSS Inc, Chicago [IL], US). A P value of
less than 0.05 was regarded as statistically significant.
Ethics approval
Ethics approval for this study was granted by the
Kowloon West Cluster Clinical Research Ethics
Committee.
Results
A total of 219 maternities with delivery
were identified during the study period. There were 221 live
births (three pairs of twins) and one stillbirth. Two (0.9%)
pregnancies had been achieved by assisted reproduction. The mean
(± SD) age of women was 29.9 ± 5.6 years. Of the 219 women, 138
(63.0%) were multiparous, 28 (12.8%) of them had had one previous
caesarean delivery, and one (0.5%) had had two previous Caesarean
sections. Overall, 139 (63.5%) women were of NE-2 category and 53
(24.2%) were of NE-3 category; the remaining 27 (12.3%) did not
provide information about their partners. A total of 138 (63.0%)
women had no booking in Hong Kong; 61 (27.9%) women had antenatal
booking in other HA hospitals; and 20 (9.1%) women were booked in
private hospitals but were referred or chose to deliver in HA
hospitals.
The reasons of admission were as follows:
show or with irregular uterine contraction (n=98, 44.7%),
suspected rupture of membranes (n=52, 23.7%), active phase of
labour (n=40, 18.3%), and antenatal complications (n=21, 9.6%;
these included 10 cases of antepartum haemorrhage, five cases of
preterm prelabour rupture of membranes, three cases of concerns on
fetal wellbeing, two cases of maternal pre-eclampsia, and one case
of threatened preterm labour). Five women admitted for postdate
pregnancy requested for delivery. Two pregnancies were delivered
in an ambulance and one on arrival to AED. One pregnancy was a
stillbirth diagnosed after admission.
Routine antenatal blood tests (complete
blood picture, blood group and Rhesus factor, immune status for
hepatitis, syphilis, rubella, and human immunodeficiency virus)
were performed in 147 (67.1%) women. For the rest of the women,
results of blood tests performed in another HA or private hospital
were available via electronic or hard copies. Ultrasound
assessment was performed for 126 (57.5%) women before delivery.
Of the 219 pregnancies, 23 (10.5%) were
delivered before 37 weeks of gestation; two (0.9%) pregnancies
were delivered after 42 weeks of gestation. A total of 141 (64.4%)
women had spontaneous onset of labour; 32 (14.6%) needed induction
of labour, and 22 (10.0%) needed augmentation of labour.
The majority of women (n=182; 83.1%) had
normal vaginal deliveries. Three (1.4%) pregnancies required
instrumental assistance. Caesarean section was performed in 13
(5.9%) pregnancies after labour and 21 (9.6%) without labour. The
success rate of trial of vaginal delivery after one previous
Caesarean section was 50%. There was no uterine scar rupture in
any case. Primary postpartum haemorrhage occurred in 13 (5.9%)
pregnancies. Seven (3.2%) women required blood transfusion. The
mean length of postnatal hospital stay was 2.0 ± 0.4 days.
Peripartum maternal complications were
divided into mild and significant. Mild complications included
seven cases of gestational hypertension, two cases of mild
pre-eclampsia without magnesium sulphate treatment, three cases of
gestational diabetes on insulin treatment, three cases of moderate
thrombocytopenia (platelet count 50-100 x 109 /L), five
cases of retained placenta requiring surgical exploration, five
cases of postpartum haemorrhage managed by medical therapy, three
cases of post-delivery urinary retention, and five cases of
postpartum fever. Significant complications included six cases of
severe pre-eclampsia requiring magnesium sulphate treatment, two
cases of placenta abruptio, two cases of major placenta praevia
type IV, one case of massive primary postpartum haemorrhage
requiring surgical intervention, and two cases of severe
thrombocytopenia (platelet count <50 x 109 /L).
During the study period, there were 121
(54.8%) male and 100 (45.2%) female live births. The mean birth
weight was 3.3 ± 0.5 kg. There were 19 (8.7%) babies with low
birth weight (<2.5 kg); 13 (5.9%) were macrosomic (>4.0 kg).
Two babies required neonatal resuscitation. The admission rates to
the NICU and special care baby unit (SCBU) were 3.7% and 43.8%,
respectively. Overall, 15 (6.8%) babies had minor congenital
abnormalities. Three (1.4%) had major abnormalities, including one
ventricular septal defect, one atrial septal defect, and one
bilateral congenital cataract. Apart from congenital problems, 51
babies had neonatal jaundice requiring phototherapy, 22 had
respiratory complications, 22 had infection episodes, five had
electrolyte disturbance, three had birth trauma, three had
congenital hypothyroidism, three had hypoglycaemia, one had
hypothermia, one had polycythaemia, one had anaemia requiring
blood transfusion, one had neonatal autoimmune thrombocytopenia
requiring intravenous immunoglobulin treatment, and one had
neurological complications. The composite neonatal morbidity rate
was 39.8%.
The pregnancy outcomes of the study cohort
were compared with the annual statistics (2011) of Kwong Wah
Hospital, as shown in Table
2. Non-local mothers were of higher
parity; more likely to have hypertensive disease (including
pre-eclamptic toxaemia), preterm delivery (<37 weeks), babies
requiring admission to SCBU, and macrosomic babies (>4.0 kg).
The rate of induction of labour and caesarean section was lower in
this group.
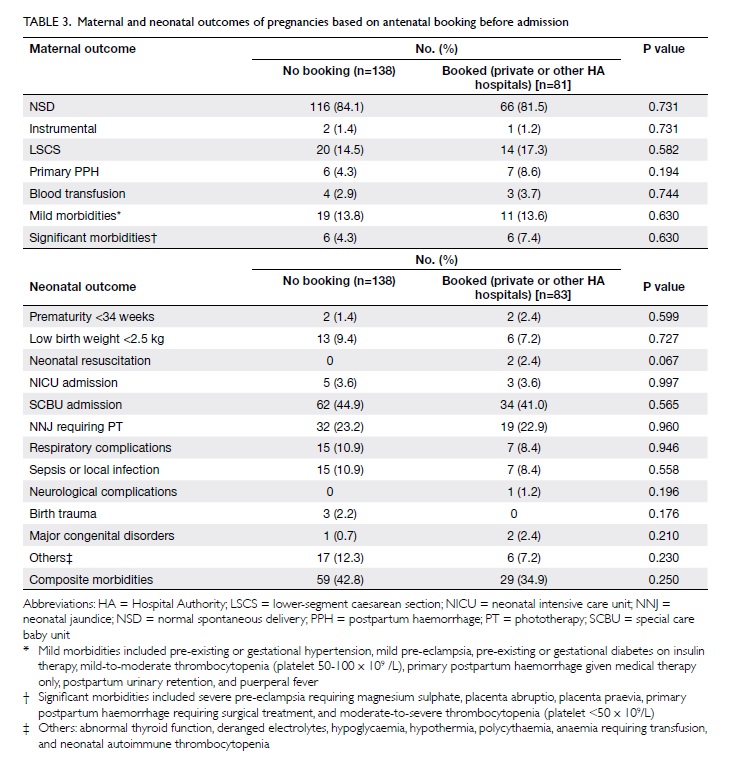
We also analysed the maternal and neonatal
outcomes based on their antenatal booking before admission (ie no
booking versus booking in other HA or private hospitals). We found
that there was no significant difference in maternal and neonatal
outcomes between the two groups. The results are shown in Table
3.
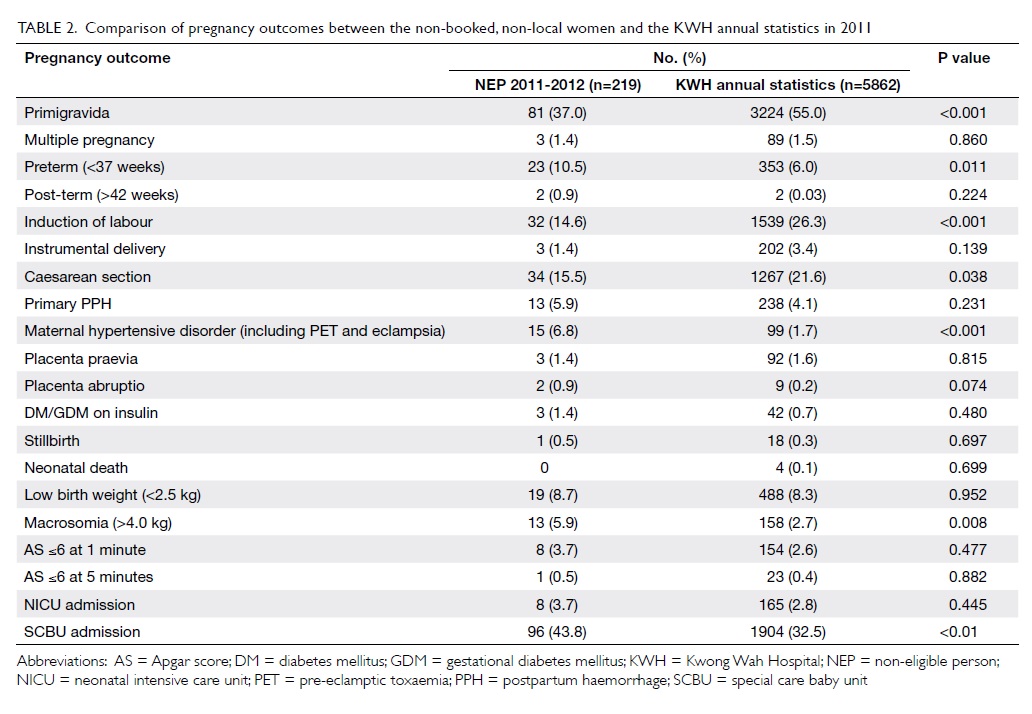
Table 2. Comparison of pregnancy outcomes between the non-booked, non-local women and the KWH annual statistics in 2011
Discussion
Standard obstetric practice is influenced
by social behaviour such as ‘birth tourism’ resulting in adverse
pregnancy outcomes; we have described this phenomenon as social
obstetrics.1 2 3 Some
women came because they wanted to evade the ‘one-child’ policy of
Mainland China. This was reflected in our study which showed that
63% of the NEP mothers were multiparous versus 45% from the
hospital annual statistics. The higher proportion of multiparity
also explained the lower rate of labour induction and caesarean
delivery in the study group. On the other hand, the significantly
higher rates of preterm delivery, hypertensive disease, macrosomic
babies, and SCBU admission suggest that the NEP mothers belonged
to a high-risk group.
In this study cohort, 63.5% of women
belonged to the NE-2 category. Their travelling permit only
allowed a short period of stay. In principle, there could be
shared care between Hong Kong and Mainland China; in reality, this
form of shared care is often suboptimal because of the differences
in clinical practice and culture between the two places. Some
mothers could not make antenatal booking in Mainland China under
the ‘one-child’ policy. Serious conditions may be detected for the
first time during an emergency admission.8
This largely endangers the health of mothers and babies. We have
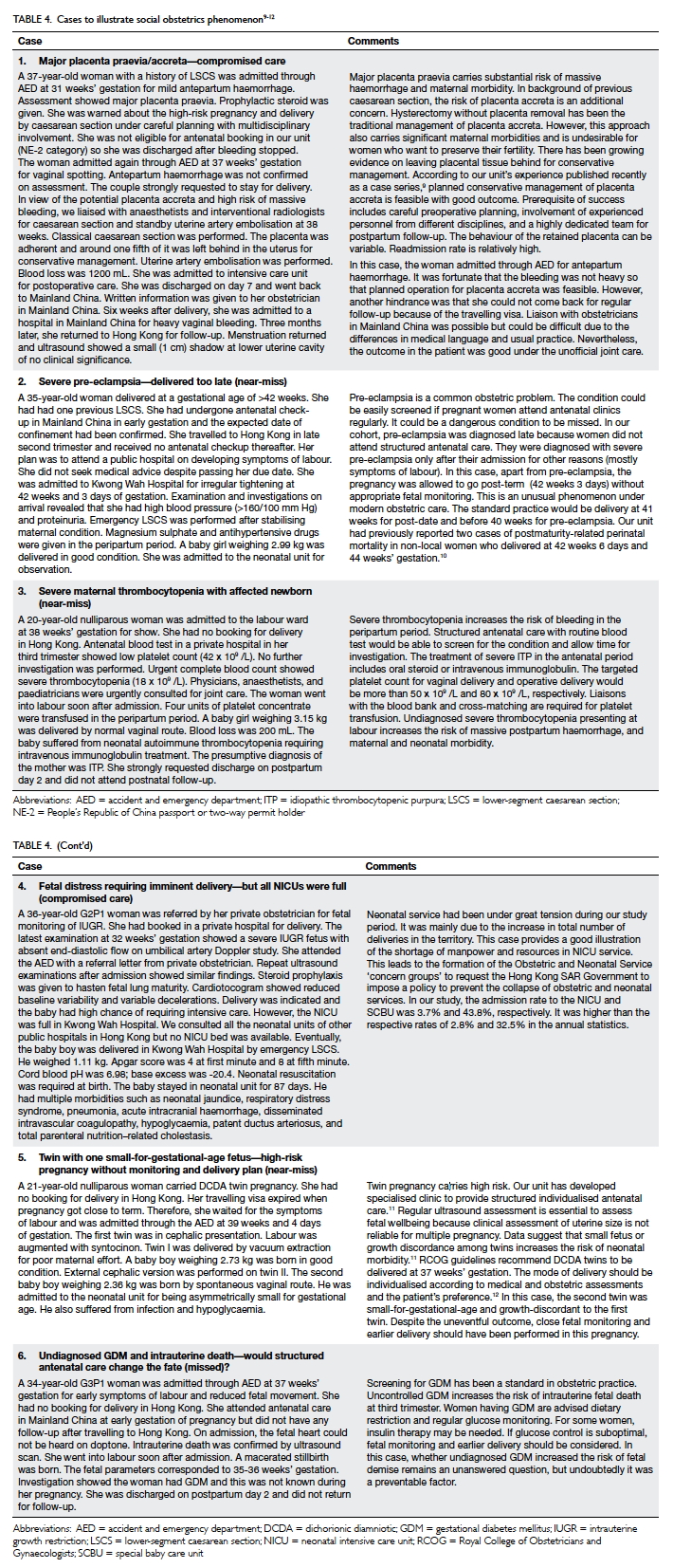
chosen six typical cases for illustrating this issue (Table
49 10 11 12).
Over the years, two local studies have been
published on the pregnancy outcomes of non-local expectant mothers
delivering in public hospitals in Hong Kong.6 7 Yuk
and Wong6 from Princess
Margaret Hospital conducted a study between 2004 and 2006 when the
HA launched the first obstetric package to the non-local women in
2005. During that period, around 35% of deliveries in Princess
Margaret Hospital were attributed to non-local Chinese women. The
proportion increased significantly from 27% in 2004 to 43% in
2006. Compared with local Chinese women, the NEPs were younger, of
lower parity, and had fewer pre-existing medical problems.
However, they had higher chances of unplanned vaginal breech
deliveries, severe hypertensive disease in pregnancy,
pre-eclampsia, delivering before arrival to hospital, and giving
birth post-term (≥42 weeks). Neonatal complications including
preterm birth, stillbirth, and neonatal death were also more
frequent among the NEP women. In fact, the first obstetric package
was proposed mainly to charge the NEPs for delivery service
expenses; it did not cover the antenatal service. This resulted in
many of them coming to the hospital only for giving birth. Many of
them came at the ‘last-minute’ to reduce the length of hospital
stay due to financial concerns. This created a heavy burden on the
public obstetric services and increased the risk of adverse
pregnancy outcomes.
The second obstetric package in 2007
encouraged the NEP mothers to receive proper antenatal checkup.
Lam7 from Tuen Mun Hospital
conducted a study from 2006 to 2008 investigating the impact of
the package on public obstetric services and pregnancy outcomes.
It was observed that the number of NEP deliveries decreased from
1868 to 1398 per year. The number of non-booked admissions through
AED reduced. The rate of post-term pregnancies dropped from 3.2%
to 1.8%. The reason for fewer deliveries was a shift of patients
to private obstetric services after setting the quota and raising
the cost. Nevertheless, this obstetric package did not improve the
admission behaviour and pregnancy outcomes.
Thanks to our HA and the Hong Kong SAR
Government’s policy of stopping NEP bookings altogether in HA
Obstetric Units, the number of NEP deliveries during our study
period (2011-2012) was significantly reduced and limited to
non-booked cases admitted through AED (Fig 2). We observed that reduction in
‘quantity’ did not improve the ‘quality’ of care in this group of
women. The admission pattern and pregnancy outcomes remained
similar to those in previous local studies. We also observed that,
although some women had prior ‘booking’ in other HA or private
hospitals, their pregnancy outcomes were no better than the ‘no
booking’ group (Table 3). One possible reason for this
could be that their travelling permit hindered them from receiving
the ‘standard’ antenatal care. It was difficult to measure the
quality of the obstetric care received by the ‘booked group’
because of its heterogeneity. We have used case examples to
illustrate how the common obstetric conditions could be
‘near-miss’ conditions or standard obstetric service could be
compromised under this social obstetrics phenomenon. We foresee
that the third obstetrics package introduced in 2012 is unlikely
to make a significant improvement in pregnancy outcomes unless the
NEP women attend a structured antenatal care like the local
mothers do.
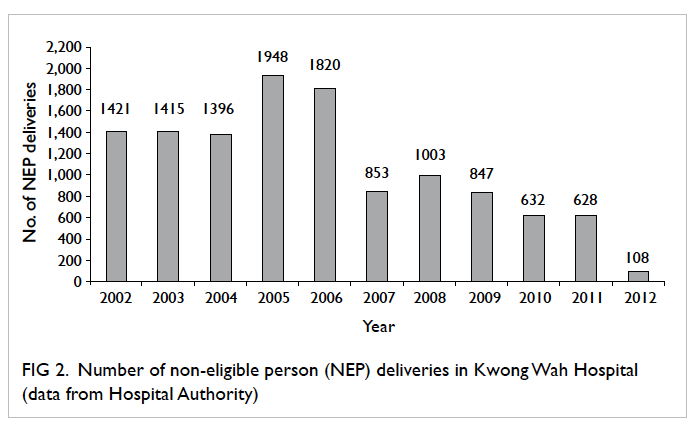
Figure 2. Number of non-eligible person (NEP) deliveries in Kwong Wah Hospital (data from Hospital Authority)
In our study, we compared the pregnancy
outcomes of our NEP cohort admitted through A&E (n=219) with
the general pregnant population from our annual statistics
(n=5862). This might introduce a pre-selection bias. Our NEP
cohort was also limited by its relatively small number. In the
study by Yuk and Wong,6 the
pregnancy outcomes of the NEP cohort (n=4657) were compared with
those of the eligible-person cohort (n=8655) from 2004 to 2006. In
the study by Lam,7 the
pregnancy outcomes of two NEP cohorts (n=1868 in 2006/2007 vs
n=1398 in 2007/2008) were compared.
Conclusion
Non-local expectant mothers delivering
babies in Hong Kong has become a classic social obstetrics
phenomenon. There is nothing wrong with these mothers who would
like to have their children to be born in Hong Kong and become
permanent residents of Hong Kong. Not long ago, Hong Kong mothers
wanted to give birth in the US or Canada so that their children
could become citizens of those countries. The problem in Hong Kong
is the large volume of pregnancies which has exceeded our
obstetric and neonatal capacities, thus affecting the health care
of our local pregnant mothers and neonates. Although our
Government now prohibits NEP bookings in both public (for NE-2 and
NE-3 categories) and private (for NE-2 category) hospitals,
non-local expectant mothers continue to admit themselves through
AED for deliveries. Health care professionals should continue to
be prepared for managing these potential near-miss clinical
situations arising from this social obstetrics phenomenon. We hope
this paper serves as one of the historical records in literature
for this social obstetrics phenomenon in the recent obstetric
history of Hong Kong.
References
1. Leung WC. Social
obstetrics—non-local expectant mothers delivering babies in Hong
Kong. The Hong Kong Medical Diary 2009;14:13-4.
2. Leung WC, Lau WL. Cross-border
families: transgression and dialogue [in Chinese]. Hong Kong: Red
Publishing; 2008: 55-9.
3. Leung WC. Social obstetrics
(cross-border pregnant women) [in Chinese]. Chiu MC, editor.
Children, medicine, law: a comparative study of Greater China.
Hong Kong: Roundtable Publishing; 2012: 40-8.
4. Au Yeung SK. Impact of
non-eligible person deliveries in obstetric service in Hong Kong.
Hong Kong J Gynaecol Obstet Midwifery 2006;6:41-4.
5. Leung TY, Lao T. Influx of
mainland expectant mothers: a blessing or a curse? Hong Kong J
Gynaecol Obstet Midwifery 2009;11:9-10.
6. Yuk JY, Wong S. Obstetrical
outcomes among non-local Chinese pregnant women in Hong Kong. Hong
Kong J Gynaecol Obstet Midwifery 2009;9:9-15.
7. Lam KD. Is the new obstetrics
package for non-local pregnant women making a change? Hong Kong J
Gynaecol Obstet Midwifery 2010;10:62-8.
8. Kwan WY, So CH, Chan WP, Leung
WC, Chow KM. Re-emergence of late presentations of fetal
haemoglobin Bart's disease in Hong Kong. Hong Kong Med J
2011;17:434-40.
9. Lo TK, Yung WK, Lau WL, Law B,
Lau S, Leung WC. Planned conservative management of placenta
accreta—experience of a regional general hospital. J Matern Fetal
Neonatal Med 2014;27:291-6. CrossRef
10. Yung C, Liu K, Lau WL, Lam H,
Leung WC, Chin R. Two cases of postmaturity-related perinatal
mortality in non-local expectant mothers. Hong Kong Med J
2007;13:231-3.
11. Yung WK, Liu AL, Lai SF, et
al. A specialised twin pregnancy clinic in a public hospital. Hong
Kong J Gynaecol Obstet Midwifery 2012;12:21-32.
12. Liu AL, Yung WK, Lai SF, et
al. Factors influencing the mode of delivery and associated
pregnancy outcomes for twins: a retrospective cohort study in a
public hospital. Hong Kong Med J 2012;18:99-107.