Hong Kong Med J 2014;20:94–101 | Number 2, April 2014 | Epub 14 Mar 2014
DOI: 10.12809/hkmj134027
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Current practices, attitudes, and perceived barriers for treating smokers by Hong Kong dentists
Kenneth WK Li, BDS1; David VK Chao, FRCGP, FHKAM (Family Medicine)2
1 Tai Po Wong Siu Ching Government Dental Clinic, 1 Po Wu Lane, Tai Po,
Hong Kong
2 Department of Family Medicine and Primary Health Care, United
Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr KWK Li (wkk_li@yahoo.com.hk)
Abstract
Objectives: To assess the attitudes of dentists
towards smoking cessation advice, as well as to
investigate their current practice and perceived
barriers to giving such advice and the relationships
among their peers regarding such activity.
Design: Cross-sectional survey.
Setting: Hong Kong.
Participants: Self-reporting questionnaires were
mailed to 330 dentists in Hong Kong by systematic
sampling. Information on their attitudes, practices,
and perceived barriers towards smoking cessation
advice and relevant background information was
collected.
Results: A total of 218 questionnaires were returned
(response rate, 66%). The majority (97%) reported
that they would enquire into every patient’s smoking
status, yet only around half of them did so routinely.
Most (95%) of the dentists who always enquired
about smoking status would actually offer smoking
cessation advice to their patients. Multiple logistic
regression of the results revealed that government
dentists (odds ratio=2.7; 95% confidence interval,
1.4-5.1), those who received training in smoking
cessation advice (2.5; 1.2-5.1), and those aged over
40 years (1.9; 1.0-3.4) were significantly more likely to enquire about smoking status. In most practices
(93%), smoking cessation advice was offered
by the dentists themselves rather than by other
team members. “Lack of training”, “unlikely to be
successful”, and “possibility of losing patients” were
the three barriers regarded as “very important” by
dentists.
Conclusions: Dentists in Hong Kong generally had
positive attitudes towards smoking cessation advice.
The dental team is in a very good position to help
smokers quit. However, training and guidelines
designed specifically for dental teams are paramount
to overcome barriers in delivering smoking cessation
advice by dental professionals.
New knowledge added by this
study
- The information gathered generally revealed a positive attitude towards delivering smoking cessation advice to smokers. However, lack of training and guidelines prevented dentists from implementing such advice in practice.
- This study raises the awareness of dentists about delivering smoking cessation advice to patients in their daily practice.
- There is a need of specific guidelines for dentists to achieve this goal.
- Practical training on such activity should be encouraged and included in both the undergraduate and postgraduate training of dentists.
Introduction
Tobacco smoking is one of the most significant public
health problems worldwide. The adverse effects of
smoking on health are well known.1 According to
the World Health Organization (WHO), the annual
death toll could rise to more than eight million by
2030, unless urgent action is taken against smoking.2
In Hong Kong, 11.1% of the population aged 15 years or above are daily smokers. Men are the
high-risk group and have a 22% prevalence of being
smokers, which is much higher than in women
(4%).3 The situation is particularly alarming, as the
smoking population is becoming younger.3 Smoking
contributes a large public health and medical burden
to society.
The Hong Kong SAR Government has implemented numerous policies and enacted
legislation on many occasions to combat tobacco
smoking. Such action has entailed raising tobacco
tax, making amendments to the existing Smoking
(Public Health) Ordinance to prohibit smoking in
public places, restricting the sale of tobacco products
and tobacco advertising. While strategies such as
taxation and prohibition of advertising are proven
to be effective, one effective strategy that should
not be ignored is “smoking cessation advice” (SCA)
delivered by health care professionals.
Smoking tobacco has been identified as
an important cause of various oral diseases and
pathologies. It is one of the most important factors
predisposing to pre-cancerous lesions and cancer of
the oral cavity, the reported pooled cancer risk being
3.4-fold higher than in non-smokers.4 It also increases
the risk of periodontal diseases,5 complications after
extractions,6 and increased rates of implant failures.7
Cross-sectional studies show that smokers have
more tooth loss.8 Other easily recognised effects
include staining of teeth,9 dental restorations, and
prosthesis10 as well as alteration of taste perception11
and halitosis.12 All these have detrimental effects
on the quality of life of smokers because of reduced
chewing efficiency, poor aesthetics, and poor self-esteem.13
The benefits of smoking cessation are
substantial. Evidence shows that smoking
counselling given by dental professions can be
effective and comparable to that offered by other
primary care professionals.14 15 16 Around a quarter of
the population have regular dental checkups and
53% have their teeth checked every 1 or 2 years.17 In
their daily practice, dental professionals have access
to a large patient population, including smokers.
Besides, the detrimental effects of smoking on the
oral cavity can be readily demonstrated directly and
thus easily appreciated by patients; this acts as a
strong motivator to quit smoking.16 Moreover, dental
treatments entailing multiple visits provide good
opportunities to motivate, reinforce, and support
smoking cessation. Thus, dental professionals
are in an excellent position for delivering advice
and counselling to smokers. Notably, counselling
by dentists has been reported to achieve an 8.6%
cessation rate after 1 year, and over 16% when also
coupled with nicotine replacement therapies.18
Despite these observations, delivery of SCA by
dentists remains less than satisfactory.19 20 21 22 According
to the literature, the reported barriers to such activity
include lack of time, resources, remuneration,
training, and fear of damaging dentist-patient
rapport.23
In Hong Kong, a study conducted in 2006
showed that more than half of all medical doctors did
not have adequate knowledge (53%) or favourable
attitudes (55%) towards smoking cessation.24 Slightly over 40% lacked confidence in delivery of SCA.
Although 77% of them obtained information on the
smoking status of their patients, only 29% advised
them to quit smoking, reflecting a low involvement
of medical doctors in the promotion of smoking
cessation.24
Local published data on the dentists’ attitudes,
practices, and barriers to delivering SCA to patients
are limited, except for one study by Lu et al.25 The
rationale of the present study was to collect data
from local dentists, and compare local results with
those gleaned from international studies.
The objectives of the present study were: (1) to
assess the attitudes of dentists towards SCA; (2) to
investigate the current practice of dentists in respect
of SCA; (3) to examine the perceived barriers to
offering SCA; and (4) to seek possible relationships
between the characteristics of dentists and their
SCA activity.
Methods
A 17-item structured, self-administered and
validated questionnaire developed by Stacey et
al26 in 2006 in the UK was adopted as the survey
instrument. The questionnaire consisted of three
main parts: (1) smoking cessation views and
activities of the dental team; (2) perceived barriers to giving SCA; and (3) perception of the importance
of the smoking cessation role of the dental team and
general medical practitioners. It was pilot-tested
with a small convenience sample (n=20) of dentists.
The target population consisted of 2026
general dentists registered with the Hong Kong
Dental Council, whose correspondence addresses
are available on a website27 that is open to the general
public. The inclusion criterion was any dentist who
was currently having a dental practice in Hong Kong
with a valid address at the time of this survey. A
systematic sample (every 6th dentists on the list) was
drawn from the 2026 registered general dentists in
Hong Kong, so as to yield the desired sample size. A
sample size of 324 subjects was calculated as needed
based on a 5% margin of error (type I error), and
95% confidence level, assuming 50% response after
distribution. Thus, 330 questionnaires were mailed
in January 2012 with stamped self-addressed reply
envelopes. Other means of reply allowed were by fax
or by online completion of the questionnaires via a
designated website. Another follow-up round of 330
questionnaires was sent to these dentists again 3
weeks after the first mailing.
Data analysis
A pilot study was carried out with a convenience
sample (n=20) to ensure the face validity of the
questionnaire. Test-retest reliability test was also
performed using these 20 subjects who were asked to
complete the questionnaire a second time (2 weeks
later). The questionnaire was viewed by three experts
in dental public health to ensure its suitability for the
present study.
All data were analysed with the Statistical
Package for the Social Sciences (Windows version
19.0; SPSS Inc, Chicago [IL], US). Frequency
distributions were generated to illustrate the
demographic data, their attitudes, practices,
and perceived barriers in SCA. To examine any
relationships between demographic variables and
outcomes, unconditional logistic regression analysis
was performed with each demographic variable
and the outcome variables (attitudes, practices,
perceived barriers). Multiple logistic regression was
then performed for variables that yielded a P value
of <0.25 in the individual analysis. The final model
contained those statistically significant variables,
using a stepwise-forward Wald logistic regression.
The significance level was set at 0.05.
Results
Response rate and demographic backgrounds
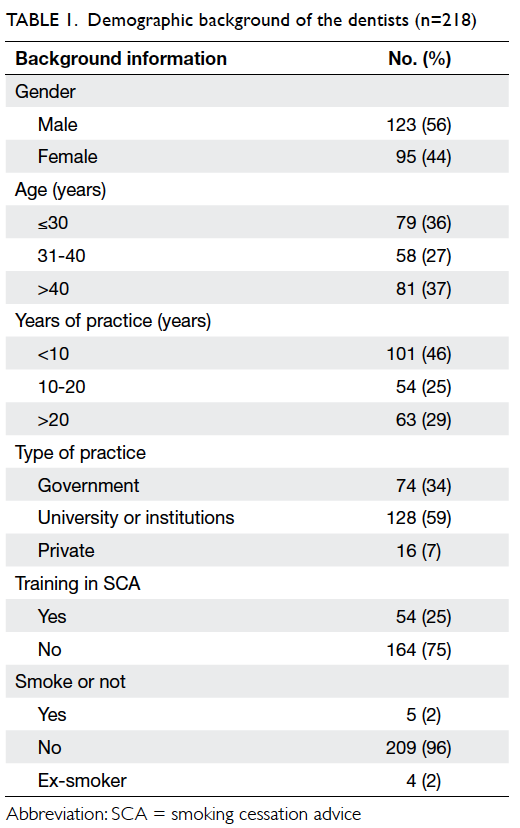
From the 330 selected dentists, 223 questionnaires
were returned (163 by mail, 39 by fax, 21 online), of
which five were incomplete. Thus, 218 questionnaires
were valid for analysis, yielding a response rate of 66%. Alarmingly, less than one fourth of the dentists
had received training in SCA. Only 16% of them had
received such training during their undergraduate
training and only 12% during postgraduate training.
Moreover, only approximately 60% of the dentists
claimed that they knew the contact of relevant
supporting agencies for SCA. Table 1 shows the
background of these dentists.
Current practices on smoking cessation
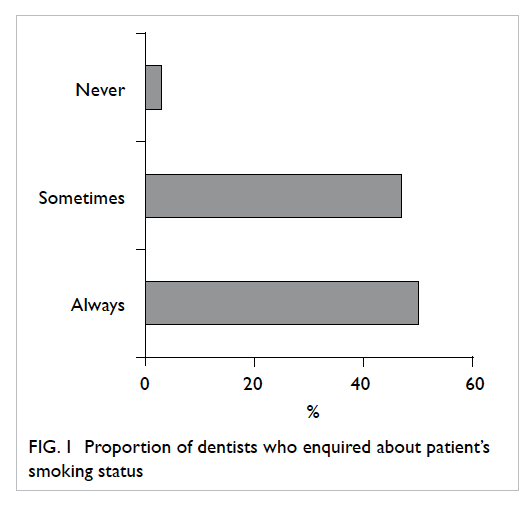
Nearly 97% of the dentists claimed that they would
enquire about their patients’ smoking status, yet
only around half of them would always do so as a
routine (Fig 1). About 97% would enquire about
smoking status whenever a patient presented with
oral diseases related to smoking (eg periodontal
disease and leukoplakia). The percentage of routine
enquiries about smoking status when patients
presented with oral white lesion (a symptom of oral
pre-cancer) was slightly higher (73%) than those
presented with periodontal disease (66%).
For dentists who would not routinely enquire
about the smoking status, around half (53%) would
always do so when patients presented with an oral
white lesion, and around 40% would do so when the
latter presented with periodontal disease.
For dentists who would always enquire about
smoking status, 95% claimed they actually offered
SCA. The majority of the dental practices (93%)
entailed SCA offered by the dentists themselves,
only 16% had dental nurses/hygienists who offered such advice and only 3% had practice managers/receptionists who did so.
After adjustments and exclusion of non-significant
variables in the unconditional logistic
regressions, only three variables were retained in
the final model and were found to be statistically
significant. These were the type of practice, receipt
of training in SCA, and age. Government dentists,
those who had received training in SCA, and those
aged over 40 years were more likely to always enquire
about their patients’ smoking status (outcome
variable of the model, P<0.05; Table 2).
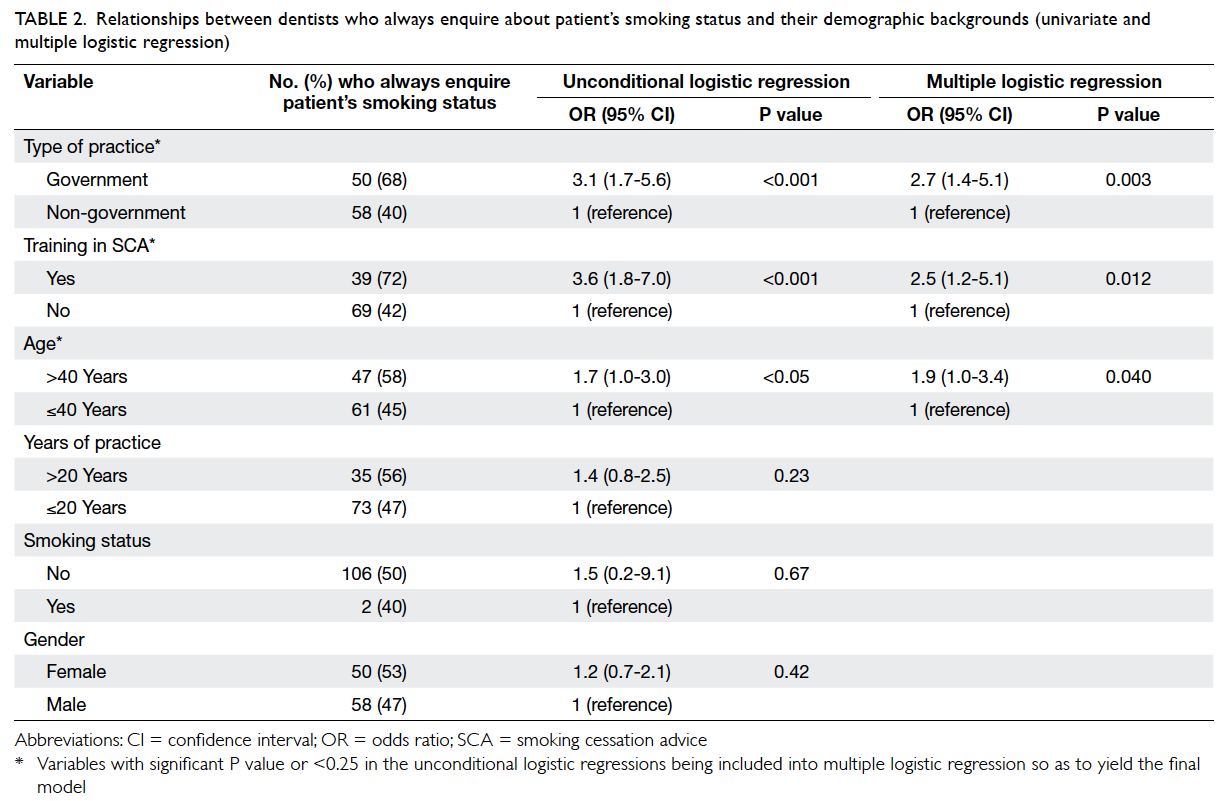
Table 2. Relationships between dentists who always enquire about patient’s smoking status and their demographic backgrounds (univariate and multiple logistic regression)
Trained dentists were more likely to always
enquire about smoking when patients presented
with periodontal disease than non-trained dentists,
the respective odds ratio (OR) and 95% confidence
interval (CI) being 3.3 and 1.5-7.2. Government
dentists were also more likely to enquire about
smoking when patients presented with a white oral
lesion (OR=2.9; 95% CI, 1.4-6.1).
Similar results prevailed with respect to
actually offering SCA to patients. Government
dentists offered such advice more often than non-government
dentists according to the logistic
regression analysis (OR=8.3; 95% CI, 1.1-64.4).
Moreover, government dentists were more likely to know how to contact supporting agencies
(OR=2.3; 95% CI, 1.1-4.6) than non-government
counterparts, and trained dentists were more
likely to know how to contact supporting agencies
(OR=14.3; 95% CI, 4.2-48.5) than those non-trained.
Attitudes and perceptions of dentists on the
role of delivering smoking cessation advice
A high proportion (89%) of dentists agreed or strongly
agreed that the dental team has an important role
in delivering SCA to patients; the percentage who
agreed or strongly agreed that medical doctors had
an important role was slightly higher (93%).
Trained dentists were 8.5 times more likely
to think that it was imperative for dental teams to
offer SCA (P<0.05). Almost all (98%) of those who
received training thought that dentists should offer
SCA, which was more than that for those who did
not have such training (86%; P=0.014).
When dentists were asked who should offer
SCA in the team, most (approximately 90%) claimed
that they should be responsible, whilst 41% thought
that nurses should also be involved, and 47% felt
that hygienists too should be involved. However,
only 16% of such personnel were actively involved
in offering SCA; the percentages were even lower for
receptionists (3%) and practice managers (1%).
Perceived barriers to delivering smoking
cessation advice by dentists
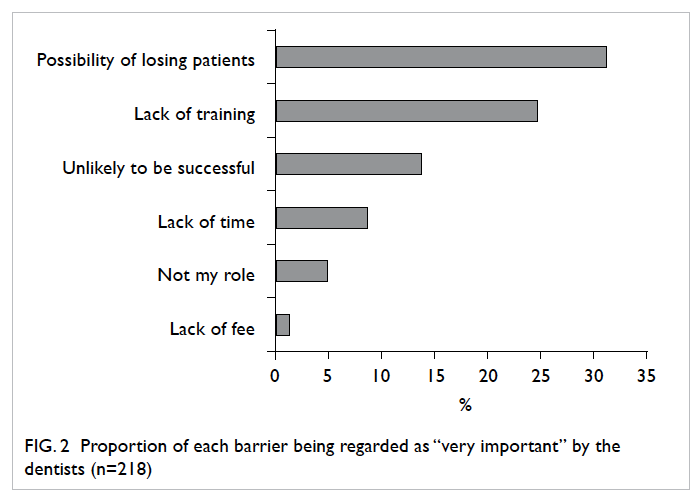
Among the potential barriers listed in the
questionnaire, the most important one identified by
the dentists was the “possibility of losing patients”
(31%), followed by the “lack of training” (25%) and
the “unlikely to be successful” (14%). On the other
hand, the “lack of time”, the “lack of fee”, and the
“not perceived as my role” were not regarded as important (Fig 2).
Discussion
This study gathered information on the current
attitudes, practices, and perceived barriers among
dentists in delivering SCA to Hong Kong patients,
which could have implications for the development
of training programmes and provide directions for
future research.
Knowledge and attitudes towards smoking
cessation advice
The present study showed that Hong Kong dentists
generally had positive attitudes and knowledge
about SCA, and recognised the adverse effects of
smoking on oral health, as reflected by the high
percentages for enquiry about a patient’s smoking
status. Moreover, nearly 90% expressed positive
attitudes towards SCA, in that they agreed it had an
important role to play.
Training and guidelines are important but
inadequate
Government dentists and dentists who received
training were significantly more likely (approximately
3 times) to routinely enquire about a patient’s
smoking status than other dentists. Trained dentists
were also approximately 14 times more likely to know
how to contact local supporting agencies, and more
than 8 times as likely to offer SCA to the patients.
They also perceived their role in offering SCA as
very important and were more actively involved
than other team members in its delivery. These
results were similar to those for Hong Kong medical
doctors,24 as well as findings of other international
and local studies.20 21 22 25
This study reflects the importance of
training and guidelines, although these were not
widely available. Only a small proportion (16%)
of dentists received training in SCA during their
undergraduate studies. Notably, for local students
the limited practical training in essential techniques
for delivering SCA to patients was similar to the
situation in the United States and Europe.28 29 Research has
shown that to increase the effectiveness of SCA,
education is needed to expand both didactic
knowledge and clinical competencies to help patients
quit smoking.30 Evidence also suggests that training
should be provided early and continued throughout
subsequent courses.31 Inclusion of both theoretical
and practical training (counselling skills, problem-solving
strategies) should be considered in future
undergraduate curricula. Moreover, continuing
professional education programmes focusing on
hands-on SCA techniques could help dentists
acquire better knowledge and more up-to-date
techniques. According to the results, the continuing education programmes should be directed towards
younger and non-government dentists.
The Department of Health has guidelines
on SCA for the government dental officers, which
includes annual updating of the patient’s smoking
status, provision of SCA, and obtaining patient
consent for referral to Tobacco Control Office when
needed. This may be one reason government dentists
were more likely to enquire about a patient’s smoking
status, offer SCA, and confirm the importance of
relevant guidelines. As in other countries, many
dentists are not familiar with guidelines like the “5A
approach”.32 Evidence suggests that dentists familiar
with guidelines are more likely to engage in SCA.33
Local information and guidelines on SCA are mostly
unclear, as they were not being designed specifically
for dentists and may not be readily accessible to
them.34 Not surprisingly, only approximately 60%
of the dentists knew how to contact supporting
agencies. Thus, clear, evidence-based, and easily
accessible guidelines designed for the dental
profession should be developed to facilitate the
effective delivery of SCA by dental professionals.
Recently, a WHO Collaborating Centre for
Smoking Cessation and Treatment of Tobacco
Dependence was set up by Department of Health. It
aims to provide evidence-based smoking cessation
training for health care personnel. It also aims
to develop, test, and evaluate models of smoking
cessation to support WHO’s initiatives on assistance
in the dissemination of relevant information on
smoking cessation. Hopefully therefore, the dental
profession will have more opportunities to receive
training in SCA in the near future.35
Barriers
Despite their apparently positive attitudes to SCA,
only around half of the dentists always enquired
about each patient’s smoking status and, if indicated,
offered SCA. These findings are consistent with
those from Australia36 and for Hong Kong medical
doctors.24 The difference in the beliefs and the
actual practice of dentists suggest barriers to
implementation. In the present study, “lack of
training”, “possibility of losing patients”, and “unlikely
to be successful” were regarded as important barriers
by the dentists, and were similar to those reported in
the UK26 and Malaysia.20 They suggest that dentists
lack confidence in delivering SCA and reinforce the
importance of adequate training. Dentists worry that
by offering SCA, they might damage relationships
with their patients. However, in reality, research
indicates that over half of the patients expect their
dentists to discuss issues related to smoking.37 Also,
such discussion could cultivate rapport between the
dentists and the patients. Thus, actually delivering
SCA could be very cost-effective in terms of gaining
patient trust. To encourage involvement of dentists in delivering SCA, efforts should be directed at
reducing the above-mentioned barriers (provision
of adequate training, informing the dentists about
current evidence, reducing their worries about
damaging relationships with patients).
Team approach
In this study, over 40% of the dentists expressed that
other personnel in their teams (nurses, hygienists)
should be involved in delivering SCA, though the
percentages were lower than those in the UK.26 Thus,
dentists generally recognised the importance of the
team approach to delivering SCA, and the literature
indicates that such team members (including
administrative staff) are in a good position to do
so.18 38 This is especially true for the hygienists, who
are responsible for managing periodontal diseases
that are smoking-related and require multiple visits,
and therefore offer excellent opportunities to deliver
SCA.39 40
The team approach should be encouraged, and
as team leader, the dentist has overall responsibility
and should actively involve other staff.41 In order to
increase the effectiveness, training of the entire dental
office team could be considered.42 The proportion of
local dentists who thought practice managers and
receptionists should be involved was low compared
to that reported from the UK.26 Variations in dental
clinic organisation in different countries may be part
of the reason; for example, locally it is not common
to involve dental practice managers in patient care.
Comparison with other studies
As mentioned previously, various aspects of our
results were generally comparable to those of other
studies. The response rate in the present study
was just under 70%, which was higher than 60%
reported from the UK,26 and 55% reported from
Malaysia,20 as well as 19% reported for Hong Kong
medical doctors24 and 50% in another study on
Hong Kong dentists.25 Our higher questionnaire
response rate could be because the questions were
simple, straightforward, and not time-consuming.
Notably, the locally developed questionnaire used by
Lu et al25 (on Hong Kong dentists) gathered more
detailed information than we did.
Limitations
The relatively low response rate in our study may
limit the generalisability of the results, and our
sample size was less than ideal. A full population
survey should be conducted if resources and time
permit. The tendency of respondents to provide
positive, favourable responses may be a source of
bias, resulting in an over-optimistic estimate of SCA
implementation. The characteristics of the non-respondents
were not known due to the anonymous nature of the questionnaire. The questionnaire was
comparatively simple, and did not address specific
aspects of knowledge on SCA, nor any specific
aspects of advice offered to patients. This limited the
scope of information being collected. Due to time
and resource limitations, other important personnel,
such as nurses and hygienists, were not surveyed.
Recommendations for future researches
A qualitative design could be considered to gain a
deeper understanding on the beliefs and barriers
to SCA with respect to the dental professions.
Thereafter an updated questionnaire could be
designed and validated, specifically for the local
setting. This could entail specific questions on
the knowledge of dentists regarding SCA and the
specific activities they and their teams undertake.
Further research could also focus on evaluating the
effectiveness of different smoking cessation training
programmes and practical approaches to SCA.
Conclusions
The present research showed that dentists in Hong
Kong generally have positive attitudes towards their
role in delivering SCA to patients. However, barriers
like the relative lack of training and guidelines,
the lack of confidence, and fear of damaging
relationships with patients may prevent them from
delivering the relevant advice. Local guidelines
specifically designed for the dental profession should
be developed and relevant resources made readily
accessible. More importantly, adequate practical
training programmes should be included in both
the undergraduate curriculum and continuing
education activities, especially for the private and
younger dentists.
References
1. World Health Organization. WHO report on the global tobacco epidemic, 2011: Warning about the dangers of tobacco. Geneva: WHO; 2011.
2. WHO key facts about tobacco. Available from: http://www.who.int/mediacentre/factsheets/fs339/en. Accessed 29 Apr 2012.
3. Census and Statistics Department, Hong Kong. General household survey and thematic household survey, 2011. Available from: http://www.census2011.gov.hk/en/index.html. Accessed Feb 2014.
4. Gandini S, Botteri E, Iodice S, et al. Tobacco smoking and cancer: a meta-analysis. Int J Cancer 2008;122:155-64. CrossRef
5. Bergstrom J. Periodontitis and smoking: an evidence-based appraisal. J Evid Based Dent Pract 2006;6:33-41. CrossRef
6. Johnson NW, Bain CA. Tobacco and oral disease. EU-Working Group on Tobacco and Oral Health. Br Dent J 2000;189:200-6.
7. Reibel J. Tobacco and oral diseases. Update on the evidence, with recommendations. Med Princ Pract 2003;12 Suppl 1:22-32. CrossRef
8. Ylöstalo P, Sakki T, Laitinen J, Järvelin MR, Knuuttila M. The relation of tobacco smoking to tooth loss among young adults. Eur J Oral Sci 2004;112:121-6. CrossRef
9. Eriksen HM, Nordbo H. Extrinsic discoloration of teeth. J Clin Periodontol 1978;5:229-36. CrossRef
10. Asmuseen E, Hansen EK. Surface discoloration of restorative resins in relation to surface softening and oral hygiene. Scan J Dent Res 1986;94:174-7.
11. Pasquali B. Menstrual phase, history of smoking and taste discrimination in young women. Percept Mot Skills 1997;84:1243-6. CrossRef
12. Rosenberg M. Clinical assessment of bad breath: current concepts. J Am Dent Assoc 1996;127:475-82. CrossRef
13. Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health–related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes 2010;8:126. CrossRef
14. Needleman IG, Binnie VI, Ainamo A, et al. Improving the effectiveness of tobacco use cessation (TUC). Int Dent J 2010;60:50-9.
15. John J. Tobacco smoking cessation counselling interventions delivered by dental professionals may be effective in helping tobacco users to quit. Evid Based Dent 2006;7:40-1. CrossRef
16. Warnakulasuriya S. Effectiveness of tobacco counseling in the dental office. J Dent Educ 2002;66:1079-87.
17. Census and Statistics Department, Hong Kong. General household survey and thematic household survey, report no. 45. Available from: http://smokefree.hk/UserFiles/resources/smoking_risk_cessation/thematic_household_surveys/THS_45Report.pdf. Accessed Feb 2014.
18. Cohen SJ, Stookey GK, Katz BP, Drook CA, Christen AG. Helping smokers quit: a randomized controlled trial with private practice dentists. J Am Dent Assoc 1989;118:41-5.
19. Allard RH. Tobacco and oral health: attitudes and opinions of European dentists; a report of the EU working group on tobacco and oral health. Int Dent J 2000;50:99-102. CrossRef
20. Ibrahim H, Norkhafizah S. Attitudes and practices in smoking cessation counselling among dentists in Kelantan. Archives of Orofacial Sciences 2008;3:11-6.
21. Uti OG, Sofola OO. Smoking cessation counseling in dentistry: attitudes of Nigerian dentists and dental students. J Dent Educ 2010;75:406-12.
22. Victoroff KZ, Dankulich-Huryn T, Haque S. Attitudes of incoming dental students toward tobacco cessation promotion in the dental setting. J Dent Educ 2004;5:563-8.
23. Watt RG, McGlone P, Dykes J, Smith M. Barriers limiting dentists' active involvement in smoking cessation. Oral Health Prev Dent 2004;2:95-102.
24. Abdullah AS, Rahman AS, Suen CW, et al. Investigation of Hong Kong doctors' current knowledge, beliefs, attitudes, confidence and practices: implications for the treatment of tobacco dependency. J Chin Med Assoc 2006;69:461-71. CrossRef
25. Lu HX, Wong MC, Chan KF, et al. Perspectives of the dentists on smoking cessation in Hong Kong. Hong Kong Dent J 2011;8:79-86.
26. Stacey F, Heasman PA, Heasman L, Hepburn S, McCracken GI, Preshaw PM. Smoking cessation as a dental intervention—views of the profession. Br Dent J 2006;201:109-13. CrossRef
27. The Hong Kong Dental Council. Lists of Registered Dentists in Hong Kong, September 2011. DCHK website: http://www.dchk.org.hk/docs/List_of_Registered_Dentists_Local.pdf. Accessed 2 Jan 2012.
28. Geller AC, Powers CA. Teaching smoking cessation in U.S. medical schools: a long way to go. Virtual Mentor 2007;9:21-5. CrossRef
29. Raupach T, Shahab L, Baetzing S, et al. Medical students lack basic knowledge about smoking: findings from two European medical schools. Nicotine Tob Res 2009;11:92-8. CrossRef
30. Ramseier CA, Christen A, McGowan J, et al. Tobacco use prevention and cessation in dental and dental hygiene undergraduate education. Oral Health Prev Dent 2006;4:49-60.
31. Brown RL, Pfeifer JM, Gjerde CL, Seibert CS, Haq CL. Teaching patient-centered tobacco intervention to first-year medical students. J Gen Intern Med 2004;19:534-9. CrossRef
32. Succar CT, Hardigan PC, Fleisher JM, Godel JH. Survey of tobacco control among Florida dentists. J Community Health 2011;36:211-8. CrossRef
33. Hu S, Pallonen U, McAlister AL, et al. Knowing how to help tobacco users. Dentists' familiarity and compliance with the clinical practice guideline. J Am Dent Assoc 2006;137:170-9. CrossRef
34. Tobacco Control Office, Department of Health, Hong Kong. Health promotion-tobacco control resources centre. Available from: http//www.tco.gov.hk/English/health/health_tcrc.html. Accessed 1 May 2012.
35. Hong Kong Council on Smoking and Health. News update—First WHO collaborating centre for smoking cessation officially launched in Hong Kong. COSH Website: http://smokefree.hk/en/content/web.do?page=news20120410. Accessed 4 May 2012.
36. Trotter L, Worcester P. Training for dentists in smoking cessation intervention. Aust Dent J 2003;48:183-9. CrossRef
37. Rikard-Bell G, Donnelly N, Ward J. Preventive dentistry: what do Australian patients endorse and recall of smoking cessation advice by their dentists? Br Dent J 2003;94:159-64. CrossRef
38. Pizzo G, Piscopo MR, Pizzo I, Giuliana G. Smoking cessation counselling and dental team [in Italian]. Ann Ig 2006;18:155-70.
39. Severson HH, Andres JA, Lichtenstein E, Gordon JS, Barckley MF. Using the hygiene visit to deliver a tobacco cessation program: results of a randomized clinical trial. J Am Dent Assoc 1998;129:993-9. CrossRef
40. Stevens VJ, Severson H, Lichtenstein E, Little SJ, Leben J. Making the most of a teachable moment: a smokeless-tobacco cessation intervention in the dental office. Am J Public Health 1995;85:231-5. CrossRef
41. Campbell HS, Sletten M, Petty T. Patient perceptions of tobacco cessation advice in dental offices. J Am Dent Assoc 1999;130:219-26. CrossRef
42. Wood GJ, Cecchini JJ, Nathason N, Hiroshige K. Office based training in tobacco cessation for dental professionals. J Am Dent Assoc 1997;128:216-24. CrossRef