Hong
Kong Med J 2018 Feb;24(1):32–7 | Epub 4 Aug 2017
DOI: 10.12809/hkmj165044
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Surgical outcome of daytime and out-of-hours surgery
for elderly patients with hip fracture
YM Chan, BSc, MSc1; N Tang, MB, ChB,
FRCSEd2; Simon KH Chow, PhD2
1 Physiotherapy Department, Pok Oi
Hospital, Yuen Long, Hong Kong
2 Department of Orthopaedics and
Traumatology, Prince of Wales Hospital, The Chinese University of Hong
Kong, Shatin, Hong Kong
Corresponding authors: Dr N Tang (ntang@ort.cuhk.edu.hk),
Dr Simon KH Chow (skhchow@ort.cuhk.edu.hk)
Abstract
Introduction: Surgery for hip
fracture may be performed out-of-hours to avoid surgical delay. There
is, however, a perception that this may constitute less-than-ideal
conditions and result in a poorer outcome. The aim of this study was to
evaluate the surgical outcome of elderly patients with hip fracture who
underwent daytime versus out-of-hours surgery in Hong Kong. This will
help make decisions about whether to operate out-of-hours or to delay
surgery until the following day.
Methods: This retrospective
study included all elderly patients with hip fracture who were operated
on and discharged from the Prince of Wales Hospital in 2014. Patients
were divided into groups according to the time of surgical incision.
Records were examined for 30-day mortality and postoperative surgical
complications, and their potential associations with surgeon
characteristics.
Results: Overall, 367 patients
were selected in this study with 242 patients in the daytime group and
125 in the out-of-hours group. Demographic characteristics were
comparable between the two groups. The overall 30-day mortality rate was
2.0% and the surgical complication rate was 24.2%. Compared with the
daytime group, there was no increase in 30-day mortality or surgical
complications for out-of-hours group. Fewer surgeons were involved in
out-of-hours surgery but the number of surgeons and their qualifications
did not affect the outcomes.
Conclusions: The two groups were
homogeneous in terms of demographic characteristics. Outcomes for 30-day
mortality and postoperative surgical complications were comparable
between the two groups. Surgeons’ qualifications and number of surgeons
involved were also not associated with the outcomes. Out-of-hours
surgery remains a viable option in order to facilitate early surgery.
New knowledge added by this study
- Time of surgery for hip fracture did not affect the outcome.
- Surgeon’s qualification was not associated with postoperative outcomes.
- Out-of-hours repair of hip fracture is safe.
- Hip operations by junior surgeons are practical.
Introduction
With the ageing population in Hong Kong, the number
of elderly people aged 65 years or above is projected to rise most rapidly
in the next 20 years, with a projected increase from 15% in 2014 to 30% in
2034.1 With this surge in the
elderly population, and as one of the most common injuries in the elderly,
hip fracture is also projected to double its numbers in 20 years.2 This places a huge financial burden on health care
resources. The sum of HK$310 million allocated to elderly patients with
hip fracture in 2011 will rise in the next few years.2
Early surgical repair is a key element both for
pain management and restoration of bone integrity after hip fracture.3 4 5 Systematic reviews show that surgery beyond 48 hours
significantly increases 30-day and 1-year mortality and complication
rates.6 7
8 9
Early surgical stabilisation and mobilisation has become the standard of
care. As a result, and due to congested operating theatre schedules,
non–life-threatening orthopaedic surgery may be performed at night.
However, there is a perception that out-of-hours surgery may result in
poorer outcomes due to insufficient technical support and surgeon fatigue
or inexperience.
Studies that investigated the effect of
out-of-hours surgery in different specialties have shown increased
morbidity and mortality risk.10 11 12
Scant literature on the effect of time of the day of operation on hip
surgery outcome shows controversial results. A German study in 200313 and a study by Chacko et al14
in 2011 showed no significant differences in mortality or complication
rate 6 months after surgery when it was performed at night. Other studies,
however, have shown that night-time surgeries for hip fracture may be
associated with increased operating time and surgical complication rate.15 16
Owing to the controversial outcomes of these
limited studies, this retrospective study aimed to evaluate the surgical
outcome of elderly patients with hip fracture who underwent surgery in
Hong Kong during the day or out-of-hours. It was hypothesised that
surgical outcomes of out-of-hours surgery would not differ significantly
to those of daytime surgery. It was hoped that findings of this study
would help surgeons in making a decision about whether to operate
out-of-hours or to delay surgery until the following day.
Methods
The Hospital Authority (HA) in Hong Kong manages
all public hospitals serving more than 90% of the population. The Clinical
Data Analysis and Reporting System (CDARS) includes in-patient data from
all hospitals and forms a huge database. The Clinical Management System
(CMS) is another computerised system that records all aspects of clinical
management in the HA.
Using these two systems, a retrospective case
series study was conducted to review individual records of patients in the
Prince of Wales Hospital (PWH) in Hong Kong. This study was approved by
the New Territories East Cluster Ethics Committee (reference number:
2015.665). Preliminary screening was performed using CDARS. All patients
discharged in 2014 with a diagnosis of hip fracture (ICD-9 code:
820.00-820.03, 820.09, 820.20-820.23 820.8, 821.00 and 905.3) and who
underwent surgical intervention (ICD-9 code: 79.15(0)-79.15(5),
79.15(7)-79.15(10)) were selected from CDARS. Records were also reviewed
through the CMS for verification. Patients aged 65 years or older with an
isolated hip fracture who underwent surgical intervention were included in
the study. Those with high-energy trauma, periprosthetic fracture,
bilateral hip fracture, or multiple lower limb fractures were excluded as
well as those with a fracture as a result of primary or metastatic bone
tumours.
Records of patients who fulfilled the criteria were
divided into two groups based on the time of surgical incision. The
daytime group included those with an operation between 08:00 and 16:59
(group 1). The out-of-hours group comprised patients of whom the procedure
was commenced between 17:00 and 07:59. This group was further split into
those having surgery before (group 2) or after midnight (group 3) to
enable more detailed analysis.
Operation procedure was defined as either fixation
or arthroplasty. Preoperative surgical risk was estimated by the American
Society of Anesthesiologists (ASA) classification. Surgeon’s qualification
was defined according to the list of specialist registration in
Orthopaedics and Traumatology in the Medical Council of Hong Kong.
Surgeons who qualified as a specialist in or before 2014 were considered a
specialist in this study. Surgery performed by a non-specialist but in the
presence of a specialist was classified as ‘non-specialist with
supervision’.
Outcome measures were 30-day mortality and
complications during hospital stay; 30-day mortality was chosen because a
shorter period could include deaths directly related to the hip surgery.
Surgical outcome was defined as complications related to surgical
procedures only. General complications such as cardiovascular,
respiratory, or cognitive complications were excluded.
Statistical analyses
Records were divided into groups based on the time
of incision. The daytime group included patients operated on between 08:00
and 16:59 (group 1). The remaining patients were assigned to the
out-of-hours group. More detailed comparison was performed with the
out-of-hours group further split into those having surgery before (group
2: 17:00 to 23:59) or after midnight (group 3: 00:00 to 07:59).
For group comparisons, continuous variables were
presented as means and standard deviations. Comparison between groups was
performed by one-way analysis of variance with post-hoc Bonferroni test.
Categorical data such as demographic data as well as mortality and
complication rates were expressed as proportion and were compared by
Pearson’s Chi squared test. Statistical analysis was performed using the
SPSS (Windows version 20.0; IBM Corp, Armonk [NY], United States). The
level of significance was set at P<0.05.
Results
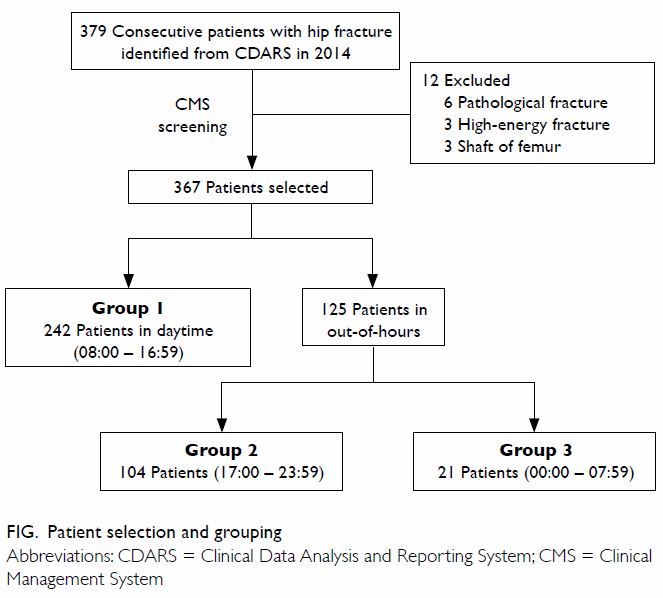
Using International Classification of Disease, 9th
revision and identified from CDARS, there were 379 hip fracture patients
operated on and discharged from PWH in 2014. Review of the related medical
records in CMS led to elimination of 12 patients according to the
inclusion and exclusion criteria. Of the remaining 367 patients, 242
patients were operated on between 08:00 and 16:59 (daytime group; group
1), and 125 patients were operated on during out-of-hours after 16:59 and
before 08:00. Among these 125 patients, 104 were operated on before
midnight (group 2: 17:00 to 23:59), and 21 were operated on after midnight
(group 3: 00:00 to 07:59). Patient selection and grouping are shown in the
Figure.
Demographic characteristics
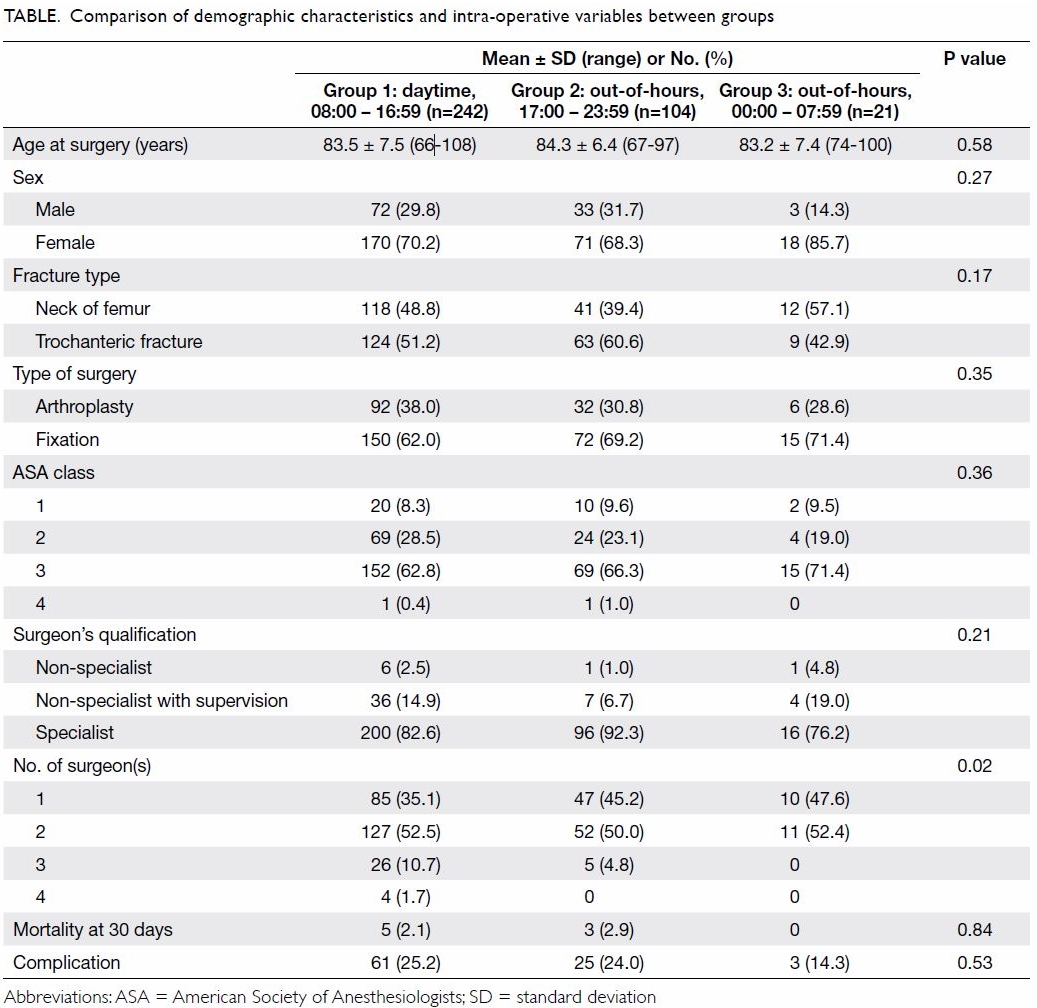
Demographic equivalency was assessed by comparing
the daytime and out-of-hours group and revealed no difference in terms of
age, sex, or type of fracture. Detailed comparison was performed with the
out-of-hours group further divided into before and after midnight as shown
in the Table. There remained no differences in terms of
age, sex, or fracture type among the groups. The mean age of the three
groups ranged from 83.2 to 84.3 years and there were more females than
males in all groups, more intertrochanteric fractures in group 1 and group
2, and more femoral neck fractures in group 3.
Intra-operative variables
Intra-operative variables were compared between the
daytime and out-of-hours groups and revealed no significant differences in
ASA class, type of surgery performed, or surgeon’s qualification. Again, a
more complete comparison was made with the three groups.
The ASA class was comparable among the groups, with
almost two thirds of the patients categorised as ASA class 3. Fixation was
more common in all the groups but the number of fixation and arthroplasty
cases was not statistically significant. There was no difference in
surgeon’s qualification among the groups, with most surgeries (>95%)
performed in the presence of a specialist. Chi squared test revealed that
significantly fewer surgeons were involved in the out-of-hours group,
especially after midnight (P=0.02).
Regarding surgical outcome, the 30-day mortality
rate and postoperative complication rate during hospital stay were
obtained. There were eight deaths among 367 patients, accounting for 2.2%
of the study population. The cause of death included chest infection and
cardiac arrest. The mortality rates were 2.1% and 2.4% in the daytime and
out-of-hours groups, respectively (P=0.84).
Surgical outcome was defined as complications
related to surgical procedure only. The overall complication rate was
24.3% in the study population with a similar rate between daytime and
out-of-hours groups. Comparable results were obtained when the
out-of-hours group was further divided into two subgroups (P=0.53). A
total of 89 patients among all groups had postoperative complications.
Fall in haemoglobin level in 89 patients required blood transfusion in
96.7% of cases. Wound infection or implant infection occurred in only four
patients. Because all patients with implant infection had revision
surgery, rate of revision surgery was the same as implant infection. No
patient had fixation failure, prosthetic dislocation, or peri-prosthetic
fracture.
Comparison of surgical time revealed no significant
difference in surgical outcome, or in surgeon’s qualification (P=0.21).
For type of surgery performed, the fixation group showed a significantly
higher surgical complication rate than the arthroplasty group (P=0.03),
although mortality rate was similar.
Discussion
Bone density insufficiency is the leading cause of
major musculoskeletal trauma following a fall in the aged population.17 In 2000, the number of hip fractures worldwide was
about 1.6 million. By 2050, the projected number will reach 4.5 million,
and more than 50% of osteoporotic hip fractures will occur in Asia.18
Encouragement of early surgery after hip fracture
will result in unavoidable out-of-hours surgery because of busy daytime
operating room schedules. Safety of surgery performed outside routine
daytime working hours, however, has long been a controversial issue.
Surgery performed after-hours may be under less-ideal conditions with
consequent poorer outcomes. This study was designed to assess if surgical
outcomes for out-ofhours surgery significantly differ to those of daytime
surgery.
In this study, patients were grouped according to
the time of surgical incision. The normal shift in the operating theatre
is 08:00 to 17:00. Surgeries performed after 17:00 and before 08:00 were
considered out-of-hours. The time period correlates with the typical
working hours and allows analysis based on a surgeon’s routine practice.
Demographic characteristics were comparable among the groups.
Outcomes of daytime and out-of-hours surgery
Mortality and complication rates were comparable
between the daytime and night-time groups. Even after midnight, when a
surgeon is thought to be most affected by fatigue, there was no
significant increase in complication rate or mortality. This was supported
by a study in 2013 that showed no significant difference in postoperative
complication rate or mortality rate after reviewing 220 dynamic hip screw
surgeries in terms of their operating time.19
It concluded that out-of-hours surgery offers the benefit of early
fixation and mobilisation, and hence may shorten the length of stay and
reduce cost of treatment.19 Chacko
et al14 also reported similar
findings in 171 hip fracture patients with surgical intervention where
mortality rate within 1 month and complication rate were comparable
between the daytime and night-time groups. Switzer et al20 studied the relationship between surgical time of day
and outcome after hip fracture fixation. They identified more than 1400
hip fracture patients with surgical intervention. Time of surgery was
treated as a continuous variable and showed no association with
complication rate at any time period. The authors concluded that there was
no difference in 30-day mortality or complications based on the time of
surgery and suggested that early operation after normal operating room
hours was safe and reasonable.20
In addition, complex cases are generally scheduled
for surgery during the daytime when more support can be obtained when
needed. This may help explain the similar surgical outcomes among the
groups. The comparable results for daytime and out-of-hours surgery shown
in this study are supported by the literature suggesting that out-of-hours
surgery is safe.
Mortality rate
The overall 30-day mortality rate was 2.2% in this
study, lower than the 3.5% to 10% reported in the UK,17 as well as the 4.96% in a 1997 local study.21 The lower mortality rate in this study may be
attributed to advancements in surgical technique and design of prostheses.
The introduction of an ortho-geriatrician in managing hip fracture
patients has also been proven to decrease mortality and complication
rates.22
Postoperative complication rate
Postoperative complications included chest
infection and acute coronary syndrome. The effect of surgeon aspects on
outcomes, however, was the main factor under investigation in this study.
Thus, surgical outcome was defined as complications related to surgical
procedure only. General complications were excluded. For surgical outcome,
fall in haemoglobin level with the need for blood transfusion, wound
infection, and implant infection were analysed.
The overall surgical complication rate was 24.2% in
this study compared with previous reports of 5% to 32% in hip fracture
fixation.15 19 20 23 24
Nonetheless, different analyses and definitions of complication rate were
used in these studies. Some studies defined complications as medical
complications or unplanned return to the operating room,15 24 whereas
others reported only wound infection, urinary tract infection, and deep
vein thrombosis.19 Thus direct
comparison with these studies was not possible. Further comparison of
blood transfusion rate with previous studies was performed, as it
represented the most common complication. The blood transfusion rate was
23.4% in this study, similar to the results in previous studies where
transfusion after hip fixation ranged from 19% to 69%.25 This may be due to incomplete reporting in the CMS as
blood transfusion was not always noted in the discharge summary. Despite
the difficulties in direct comparison of the complication rate with
previous study, we suggest that the rate in this study was reasonable.
Number and qualification of surgeons
Significantly fewer surgeons were involved in
out-of-hours surgery. This may be because training of junior staff
commonly occurs during the daytime. Although fewer surgeons were involved
in out-of-hours surgeries, this may be compensated by the experience of
the surgeon since a larger proportion of out-of-hours surgeries was
performed by a specialist. Nonetheless, the difference was not
significant.
Furthermore, the qualification of the surgeon had
no association with surgical outcomes in this study. This may be because
cases were screened prior to allocation. Difficult and more complex cases
would likely be operated on by a more experienced surgeon. Holt et al26 showed comparable results in their study of the
Scottish Hip Fracture Audit Database published in 2008. They studied more
than 18 000 patients and concluded that grade of surgeon did not
significantly affect surgical outcome.26
Strengths and limitations
This is the first local study based in a major
hospital in Hong Kong to analyse the effect of operating time on surgical
outcome. The out-of-hours group was split into before and after midnight
so as to focus on surgeon fatigue. Analysis of surgeon expertise revealed
that surgical outcome was not compromised by surgeon’s qualification.
There are several limitations in this study. First,
this was a retrospective study with no functional outcomes. Information on
complications was retrieved from the CMS only which might not have
recorded all complications. A fracture registry or prospective study with
more representative complications including prosthetic dislocation,
peri-prosthetic fracture, implant loosening, fixation failure,
malreduction, malfixation, and implant malposition is suggested in future.
Data collection was performed by the authors who were not blinded so this
might have introduced bias. Blood transfusion, the most common
complication reported, was believed to be related to the operative
procedure. Fall in haemoglobin level due to other causes, however, could
not be excluded simply from details in the CMS. Second, the overall
population size and the relatively smaller number of cases in the
after-midnight group might not have the statistical power to show any
difference. Further study with a larger sample size is suggested. Finally,
several potential confounders were not investigated, for example,
fractures were not classified according to stability and time to surgery.
These factors may be associated with poorer outcome.
Conclusion
This study demonstrates similar outcomes of elderly
patients with hip fracture in terms of mortality and postoperative
complications for daytime and out-of-hours surgery. Qualification and
number of surgeons involved were not associated with outcome. To
facilitate better outcome with early operation, out-of-hours surgery
remains a safe option and the only means to overcome limited resources.
Declaration
All authors have disclosed no conflicts of
interest.
References
1. Hong Kong population projections
2015-2064. Census and Statistics Department, the Government of the Hong
Kong Administrative Region. Available from:
http://www.statistics.gov.hk/pub/B1120015062015XXXXB0100.pdf. Accessed Dec
2015.
2. Ngai WK. Fragility Fracture Registry in
Hong Kong. Proceedings of the Hospital Authority Convention 2014; 2014 May
7-8; Hong Kong.
3. Mak JC, Cameron ID, March LM; National
Health and Medical Research Council. Evidence-based guidelines for the
management of hip fractures in older persons: an update. Med J Aust
2010;192:37-41.
4. Australian & New Zealand Hip
Fracture Registry. Australian and New Zealand guideline for hip fracture
care. September 2014.
5. Evidence update—Hip fracture. London:
National Institute for Health and Clinical Excellence. March 2013.
6. Shiga T, Wajima Z, Ohe Y. Is operative
delay associated with increased mortality of hip fracture patients?
Systematic review, meta-analysis, and meta-regression. Can J Anaesth
2008;55:146-54. Crossref
7. Sircar P, Godkar D, Mahgerefteh S,
Chambers K, Niranjan S, Cucco R. Morbidity and mortality among patients
with hip fractures surgically repaired within and after 48 hours. Am J
Ther 2007;14:508-13. Crossref
8. Siegmeth AW, Gurusamy K, Parker MJ.
Delay to surgery prolongs hospital stay in patients with fractures of the
proximal femur. J Bone Joint Surg Br 2005;87:1123-6.Crossref
9. Simunovic N, Devereaux PJ, Sprague S, et
al. Effect of early surgery after hip fracture on mortality and
complications: systematic review and meta-analysis. CMAJ 2010;182:1609-16.Crossref
10. Desai V, Gonda D, Ryan SL, et al. The
effect of weekend and after-hours surgery on morbidity and mortality rates
in pediatric neurosurgery patients. J Neurosurg Pediatr 2015;16:726-31. Crossref
11. Kelz RR, Freeman KM, Hosokawa PW, et
al. Time of day is associated with postoperative morbidity: an analysis of
the national surgical quality improvement program data. Ann Surg
2008;247:544-52. Crossref
12. Scott SW, Bowrey S, Clarke D, Choke E,
Bown MJ, Thompson JP. Factors influencing short- and long-term mortality
after lower limb amputation. Anaesthesia 2014;69:249-58. Crossref
13. Dorotka R, Schoechtner H, Buchinger W.
Influence of nocturnal surgery on mortality and complications in patients
with hip fractures [in German]. Unfallchirurg 2003;106:287-93. Crossref
14. Chacko AT, Ramirez MA, Ramappa AJ,
Richardson LC, Appleton PT, Rodriguez EK. Does late night hip surgery
affect outcome? J Trauma 2011;71:447-53; discussion 453. Crossref
15. Bhattacharyya T, Vrahas MS, Morrison
SM, et al. The value of the dedicated orthopaedic trauma operating room. J
Trauma 2006;60:1336-40. Crossref
16. Wixted JJ, Reed M, Eskander MS, et al.
The effect of an orthopedic trauma room on after-hours surgery at a level
one trauma center. J Orthop Trauma 2008;22:234-6. Crossref
17. Giannoulis D, Calori GM, Giannoudis
PV. Thirty-day mortality after hip fractures: has anything changed? Eur J
Orthop Surg Traumatol 2016;26:365-70. Crossref
18. Poh KS, Lingaraj K. Complications and
their risk factors following hip fracture surgery. J Orthop Surg (Hong
Kong) 2013;21:154-7. Crossref
19. Rashid RH, Zubairi AJ, Slote MU,
Noordin S. Hip fracture surgery: does time of the day matter? A
case-controlled study. Int J Surg 2013;11:923-5. Crossref
20. Switzer JA, Bennett RE, Wright DM, et
al. Surgical time of day does not affect outcome following hip fracture
fixation. Geriatr Orthop Surg Rehabil 2013;4:109-16. Crossref
21. Ho ST, Chau YS, Wong WC. Short-term
outcome of operated geriatric hip fracture. Hong Kong J Orthop Surg
1997;1:7-12.
22. Vidán M, Serra JA, Moreno C, Riquelme
G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older
patients hospitalized for hip fracture: a randomized, controlled trial. J
Am Geriatr Soc 2005;53:1476-82. Crossref
23. Zuckerman JD, Skovron ML, Koval KJ,
Aharonoff G, Frankel VH. Postoperative complications and mortality
associated with operative delay in older patients who have a fracture of
the hip. J Bone Joint Surg Am 1995;77:1551-6. Crossref
24. Lawrence VA, Hilsenbeck SG, Noveck H,
Poses RM, Carson JL. Medical complications and outcomes after hip fracture
repair. Arch Intern Med 2002;162:2053-7. Crossref
25. Liodakis E, Antoniou J, Zukor DJ, Huk
OL, Epure LM, Bergeron SG. Major complications and transfusion rates after
hemiarthroplasty and total hip arthroplasty for femoral neck fractures. J
Arthroplasty 2016;31:2008-12. Crossref
26. Holt G, Smith R, Duncan K, Finlayson
DF, Gregori A. Early mortality after surgical fixation of hip fractures in
the elderly: an analysis of data from the scottish hip fracture audit. J
Bone Joint Surg Br 2008;90:1357-63. Crossref