Hong Kong Med J 2017 Aug;23(4):365–73 | Epub 7 Jul 2017
DOI: 10.12809/hkmj165043
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
A cross-sectional study of the knowledge, attitude, and
practice of patients aged 50 years or above towards herpes zoster in an
out-patient setting
Anthony CY Lam, MY Chan, HY Chou, SY Ho, HL Li, CY
Lo, KF Shek, SY To, KK Yam, Ian Yeung
Li Ka Shing Faculty of Medicine, The
University of Hong Kong, Pokfulam, Hong Kong
Corresponding author: Anthony CY Lam (hrp20152016@gmail.com)
Abstract
Introduction: There has been
limited research on the knowledge of and attitudes about herpes zoster
in the Hong Kong population. This study aimed to investigate the
knowledge, attitude, and practice of patients aged 50 years or above
towards herpes zoster and its vaccination.
Methods: This was a
cross-sectional study in the format of a structured questionnaire
interview carried out in Sai Ying Pun Jockey Club General Outpatient
Clinic in Hong Kong. Knowledge of herpes zoster and its vaccination was
assessed, and patient attitudes to and concerns about the disease were
evaluated. Factors that affected a decision about vaccination against
herpes zoster were investigated.
Results: A total of 408 Hong
Kong citizens aged 50 years or above were interviewed. Multiple
regression analysis revealed that number of correct responses regarding
knowledge about herpes zoster was positively correlated with educational
attainment (B=0.313, P=0.026) and history of herpes zoster (B=0.408,
P=0.038), and negatively correlated with age (B= –0.042,
P<0.001) and male gender (B= –0.396, P=0.029). Answers
to several questions revealed a sizable number of misconceptions about
the disease. Among all respondents, 35% stated that they were worried
about getting the disease, and 17% would consider vaccination against
herpes zoster.
Conclusions: Misconceptions
about herpes zoster were notable in this study. More health education is
needed to improve the understanding and heighten awareness of herpes
zoster among the general public. Although the majority of participants
indicated that herpes zoster would have a significant impact on their
health, a relatively smaller proportion was actually worried about
getting the disease. Further studies on this topic should be encouraged
to gauge the awareness and knowledge of herpes zoster among broader
age-groups.
New knowledge added by this study
- Certain misconceptions about herpes zoster persist among Hong Kong people.
- While a majority of participants indicated that herpes zoster would have a significant impact on their health, a relatively smaller proportion of respondents were actually worried about getting the disease.
- Vaccination against herpes zoster is currently not common among Hong Kong people.
- More health education should be provided to improve knowledge about herpes zoster and clarify misconceptions about the disease among Hong Kong people.
- Health promotion that includes treatment and/or prevention of herpes zoster can be explored.
Introduction
Varicella zoster virus (VZV) is a member of the
Herpesviridae family and is an enveloped double-stranded DNA virus.
Primary infection with VZV causes varicella, commonly known as chickenpox.
The virus migrates to the sensory ganglia and establishes latency, by
which the affected individual becomes asymptomatic. Reactivation of the
virus causes herpes zoster (HZ), also known as shingles.1
Infection with VZV is the highest reported
notifiable infectious disease in Hong Kong, with 8879 cases reported in
2016.2 A study
in 1994 showed that antibodies against VZV were found in more than 90% of
children by 8 years of age,3
illustrating that latent infection was highly prevalent. These individuals
would be at risk of HZ.
Studies report the lifetime prevalence of HZ to be
approximately 10% to 32%.1 4
The University of Hong Kong estimated the prevalence of HZ to be 16.8%.5
The incidence of HZ is positively correlated with age.6
Individuals who are immunocompromised7 or have a chronic
disease8 may be at a greater risk of having HZ.
The viral disease HZ presents with a rash with dermatomal distribution,
accompanied by vesicular eruption and neuropathic pain.7
A number of complications can result from HZ.9
Post-herpetic neuralgia, a persistent neuropathic pain in the area
affected by HZ, can develop particularly in older adults.9 10
Other serious sequelae include HZ ophthalmicus, HZ oticus and bacterial
skin infections, all of which adversely affect the quality of life of
patients.9 These also place a significant economic
burden on the health care system.11 In 2009, a study
estimated the cost of treating new HZ cases in the US to be
over one billion US dollars each year.12 Active HZ can
be treated by antiviral therapy, such as acyclovir.7 13
The vaccine for HZ is a live vaccine approved by the Food and Drug
Administration (FDA) of the US in 2006 for the prevention of HZ
in immunocompetent patients aged 60 years or above.14
The vaccine has been approved for use in Hong Kong since 2007.13
The FDA approved the use of the vaccine in individuals aged 50 to 59 years
in 2011.15 According to the Shingles
Prevention Study,16 HZ vaccine lowered the incidence of
HZ by 51% and reduced the pain and discomfort of postherpetic neuralgia by
66% when compared with placebo. Similar studies to assess public awareness
of HZ and its vaccination were then carried out. The Herpes Zoster Global
Awareness Survey from 22 countries17 and a knowledge,
attitude, and practice study in South Korea18 were conducted in 2009 and
2015, respectively. Factors promoting or limiting the prevalence of
vaccination against HZ were also investigated in the latter study.18
There has been limited research conducted in the Hong Kong population to
assess the knowledge of and attitudes towards HZ and the practice of
vaccination. This study aimed to explore these areas.
Methods
Setting and participants
A cross-sectional survey was conducted in 11 clinic
sessions during 24 July to 12 August 2015 at the Sai Ying Pun Jockey Club
General Outpatient Clinic (GOPC). The GOPC is open to the general public
and serves all patients who comprise mainly those with chronic or episodic
disease. There were 6330 patients attending the clinic during the study
period, of which approximately three quarters aged 50 years or above.
These patients in the waiting area of the clinic were selected by
convenience sampling to participate in this study. No additional criteria
were set to allow for a higher degree of generalisability. Participants
were asked to complete a face-to-face questionnaire after giving written
informed consent. They were allowed to either complete the questionnaire
themselves, or listen to the researcher reading the questions aloud
without any additional interpretation, then answer the question verbally.
Approval was obtained from the Institutional Review Board of the
University of Hong Kong/Hospital Authority Hong Kong West Cluster and the
GOPC prior to commencement of this study.
Research instrument
A questionnaire consisting of 30 items was
designed; this included questions on demographics (n=3), medical history
(n=4), whether the respondent had heard about HZ (n=1), knowledge of HZ
(n=8) and HZ vaccination (n=6); attitudes towards preventing HZ (n=7);
and whether the respondent would consider vaccination against HZ (n=1).
Statistical analysis
To estimate the proportions of participant
responses to the questions about knowledge of HZ, for 95% confidence
level with an expected true proportion of 50% and 5% margin of error, a
sample size of 385 was obtained using the formula:
N=Z2p(1−p)/C2
where N=sample size, Z=Z value, p=population variance, and C=margin of error
N=Z2p(1−p)/C2
where N=sample size, Z=Z value, p=population variance, and C=margin of error
To analyse the number of correct responses associated with five
demographic factors with an effect size (f2)
of 0.15 and a statistical power of 0.8, an a-priori analysis was
employed to obtain the sample size of 92 to achieve a 5% margin of
error, using G*Power (version 3.1.9.2) and the following formulae19:
N=λ/f2 and N=v+u+1
where N=sample size, λ=non-centrality parameter, f2=effect size, v=degree of freedom of the denominator of the F ratio, and u=number of predictors
N=λ/f2 and N=v+u+1
where N=sample size, λ=non-centrality parameter, f2=effect size, v=degree of freedom of the denominator of the F ratio, and u=number of predictors
Statistical analysis was performed with SPSS (Windows version 23.0; IBM
Corp, Armonk [NY], US). Demographic data, medical history, respondents’
attitude towards preventing HZ and decision about HZ vaccination were
analysed by descriptive statistics. Regarding knowledge of HZ, the
number of correct responses out of eight questions was calculated.
Multiple linear regression analysis was used to evaluate the association
of the number of correct responses with age, gender, educational
attainment, history of HZ, and history of chronic diseases. Chi squared
tests were applied to evaluate the associations in giving correct
response to each question among the same five variables. A P value of
<0.05 was considered significant.
Results
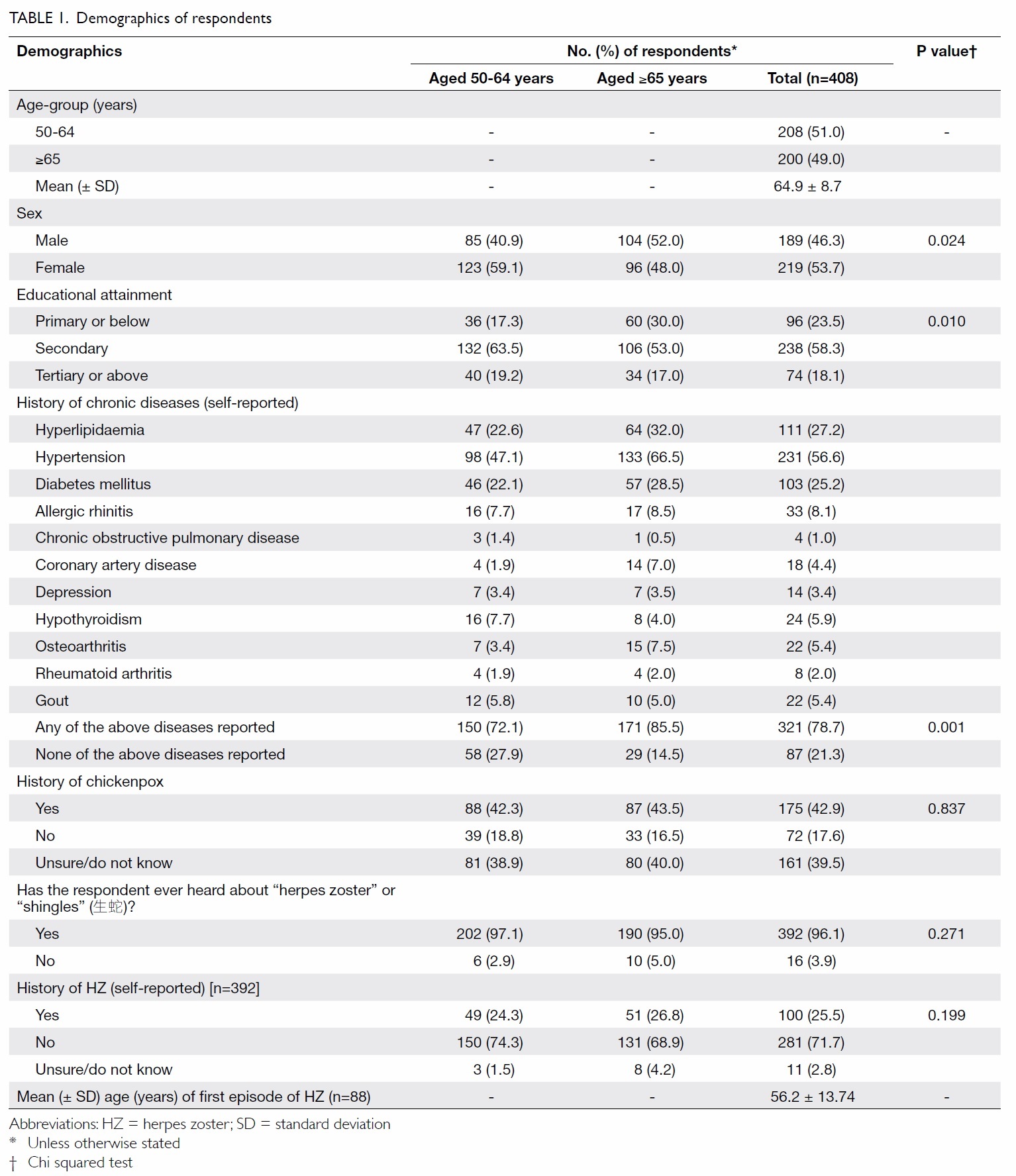
Demographics
A total of 496 persons were invited to
participate in the study, of whom 430 agreed which corresponded to a
response rate of 87%; 408 valid responses were collected. The sample was
not weighted by the population because the male-to-female ratio was
similar to that of the population (48:52).20 The
demographic data are shown in Table 1. Approximately 40% of respondents did not know their history of
chickenpox despite its high prevalence, whereas over 95% had heard of
the condition of HZ. Although some respondents did not understand the
medical terminology “herpes zoster”, most of them knew the Cantonese
colloquial name (生蛇).
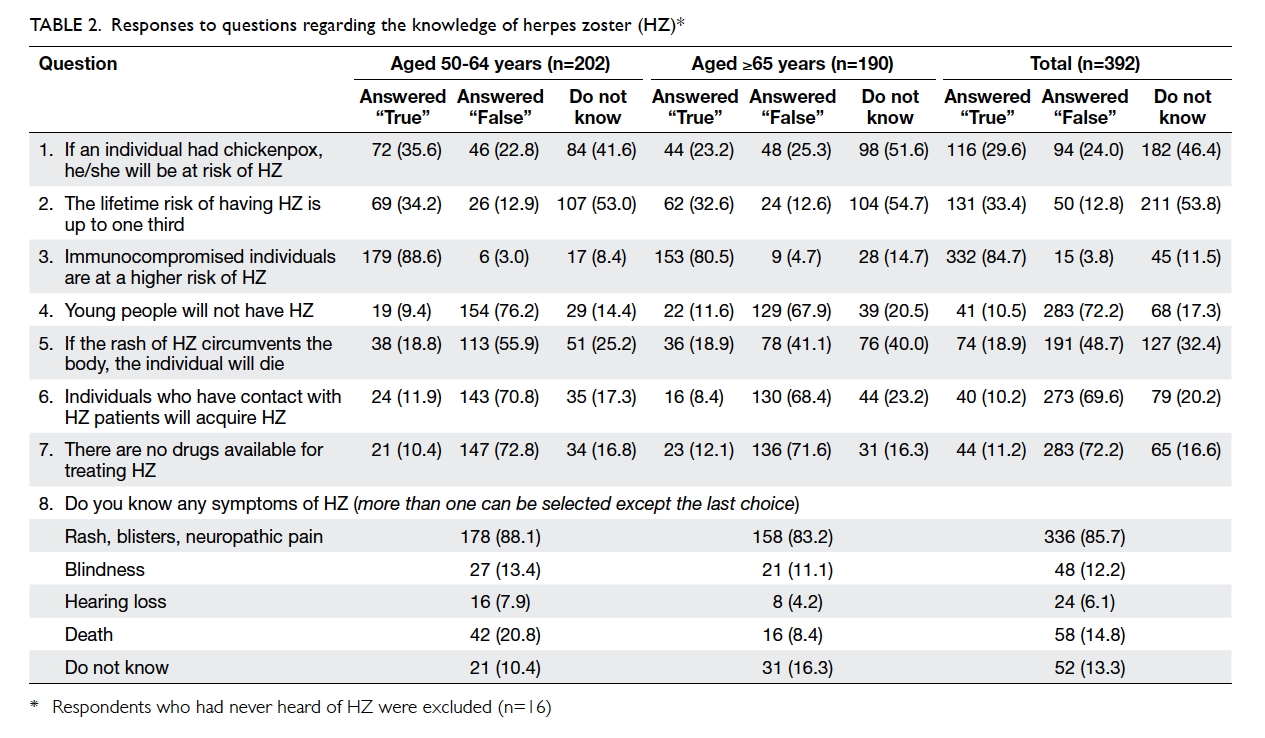
Knowledge of herpes zoster
Table 2 summarises the responses to the eight questions pertaining to
the knowledge of HZ, in which 16 respondents who had never heard of the
condition were excluded. Only 29.6% knew that chickenpox and HZ are
related. Over half were unsure of the lifetime prevalence of HZ.
Immunocompromised state was a well-known risk factor of HZ (84.7%).
Over 70% were aware that VZV can reactivate in young ages.
Rash, blisters, and neuropathic pain were the most commonly known
symptoms of HZ, identified by 85.7% of respondents. Nonetheless 13.3%
did not know the symptoms of HZ even though they had heard of the
disease.
There is a saying in Chinese society that death will ensue when the rash
of HZ circumvents the body. Worryingly, only slightly less than half
(48.7%) knew that this was untrue, 18.9% thought the statement was true
and the remaining were unsure. Additionally, 69.6% gave the correct
response that contacts of HZ patients could not acquire HZ infection
directly, and 72.2% knew that HZ was treatable.
Respondents scored a mean (±standard deviation [SD]) of 4.96 (±1.72) correct responses out of eight. Over half of all subjects answered five or
six questions correctly.
Of 392 participants who had heard of HZ, 11 respondents who were uncertain
of their history of HZ were excluded from the multivariate regression
analysis regarding the knowledge of HZ (Table
3a). The number of correct responses was positively correlated with
educational attainment (P=0.026) and history of HZ (P=0.038), but
negatively correlated with age per year (P<0.001) and male gender
(P=0.029).
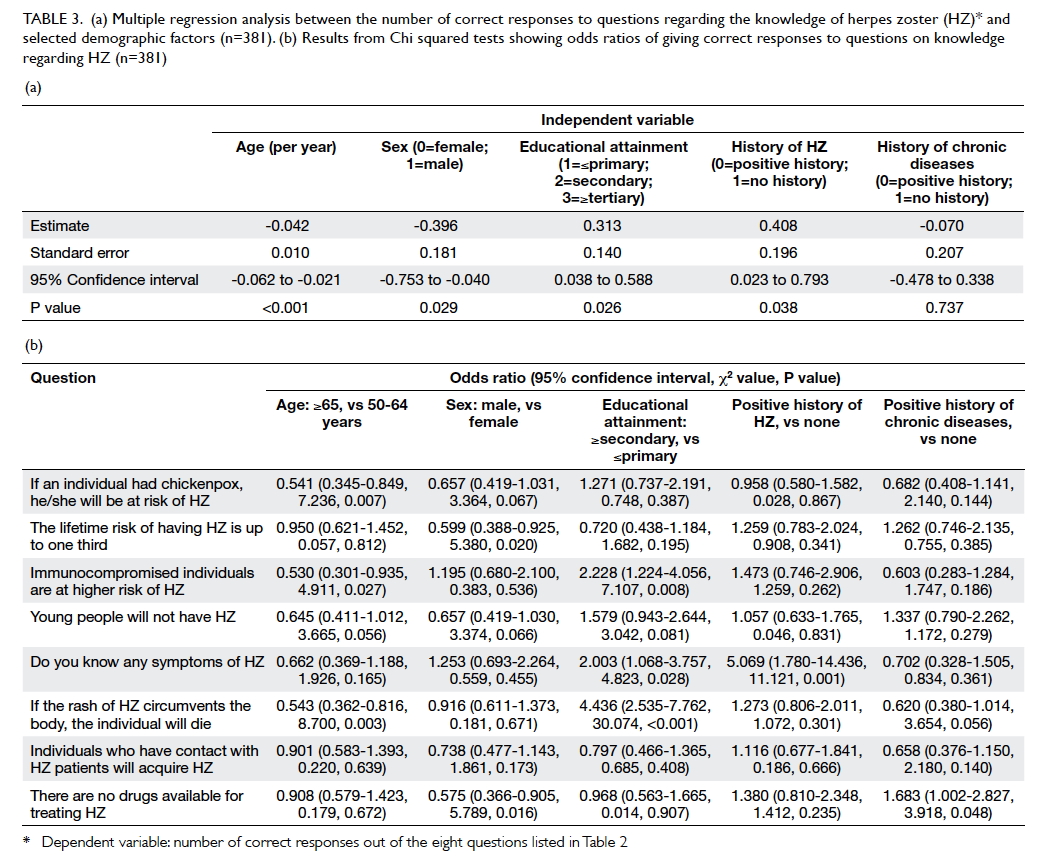
Table 3. (a) Multiple regression analysis between the number of correct responses to questions regarding the knowledge of herpes zoster (HZ) and selected demographic factors (n=381). (b) Results from Chi squared tests showing odds ratios of giving correct responses to questions on knowledge regarding HZ (n=381)
The results of the Chi squared tests and the corresponding odds ratios are
shown in Table 3b. Respondents aged 65 years or above were half as likely as those
aged 50-64 years to give correct responses regarding the relationship
between chickenpox and HZ (P=0.007), the higher risk of HZ among
immunocompromised individuals (P=0.027), and the misconception of death
associated with a circumventing rash (P=0.003). In contrast,
participants with higher educational attainment were more likely than
those without to give appropriate answers to the latter two questions
(P=0.008 and P<0.001, respectively).
Respondents with a history of HZ (P=0.001) and those with higher
educational attainment (P=0.028) were more likely to correctly identify
the symptoms of HZ.
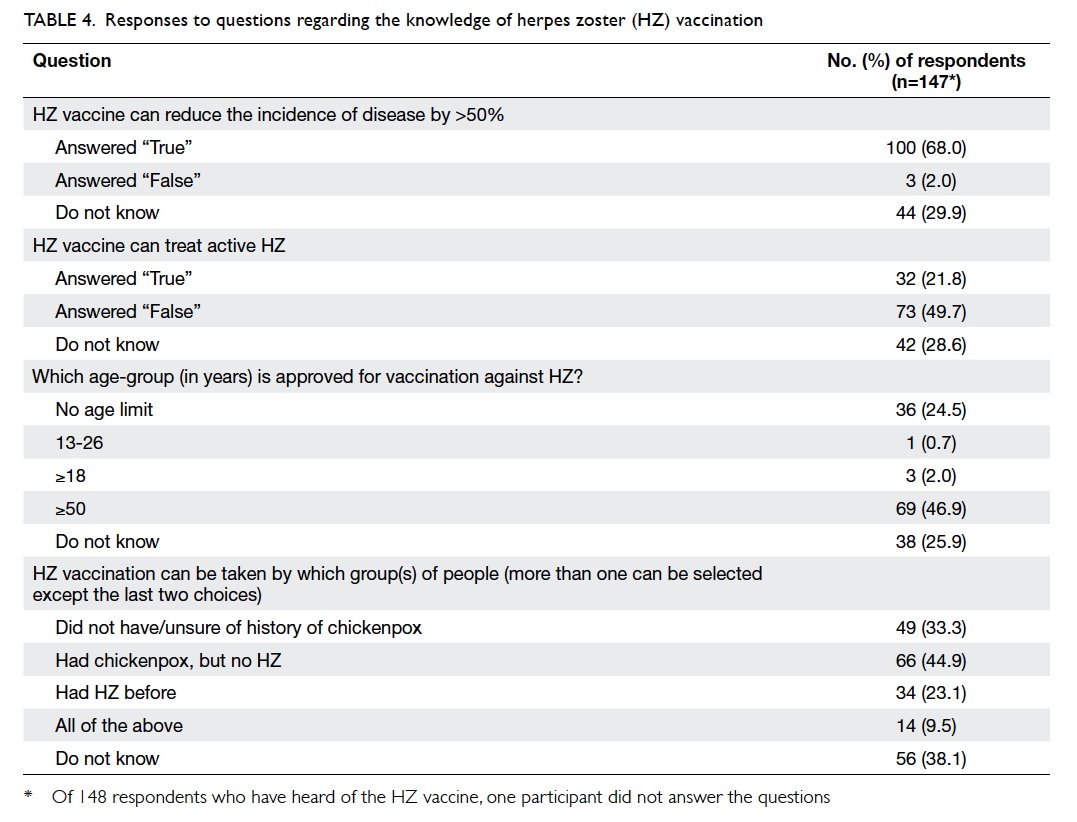
Knowledge of herpes zoster vaccination
Of 392 respondents, 148 (37.8%) had heard of the
HZ vaccine. Only this subgroup was asked to answer four additional
questions about the vaccine (Table
4). One respondent who did not answer the questions was excluded. On
average, 1.73 (±1.00) out of four responses were correct.
Nearly half of these respondents (46.9%) correctly identified the target
age-group for HZ vaccination and 24.5% thought there was no age limit.
Most subjects did not know that vaccination is possible regardless of
history of chickenpox or HZ. Around two thirds (68.0%) were aware that
the vaccine can significantly reduce the incidence of HZ, but only 49.7%
knew that the vaccine is not indicated for treatment of active disease.
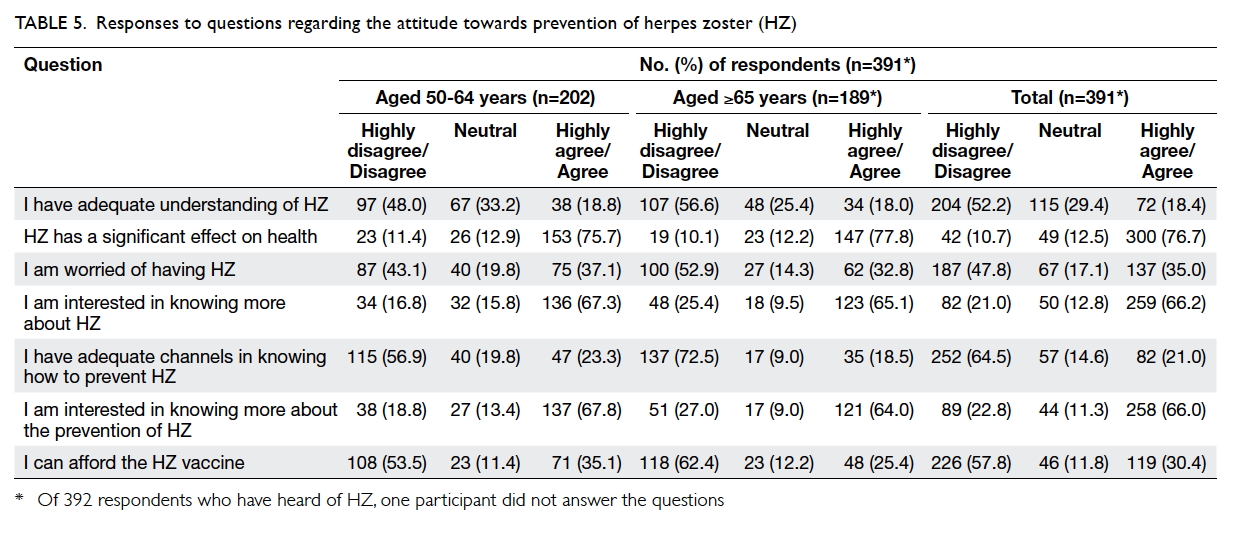
Attitudes and practice
Table
5 gives a breakdown of the seven questions about attitudes of
respondents to HZ. Over half (52.2%) of 391 respondents (with one
participant who did not answer the questions being excluded) thought
they had an insufficient understanding of HZ. Almost two thirds were
interested in learning more about the disease (66.2%) and its prevention
(66.0%). A similar percentage of subjects (64.5%) remarked that there
were inadequate channels to learn about prevention of the disease. While
76.7% believed that HZ could affect their health significantly, only
35.0% were worried about getting the disease. Almost one third (30.4%)
said that they could afford the HZ vaccine.
Among the subgroup who had heard of the HZ vaccine, 140 (94.6%) replied
that their doctor had not mentioned or recommended the vaccine.
This study compared the vaccination rate for HZ with that of influenza
and pneumococcus. The latter two vaccines are recommended by the Centre
for Health Protection for those aged above 65 years and are included in
the Elderly Vaccination Subsidy Scheme.21 Enquiry
revealed that 26.9% and 14.3% of 391 respondents had taken the influenza
vaccine in the past year and pneumococcal vaccine in the past 5 years,
respectively. The figures were much higher than that for HZ vaccination
(2.8%).
When asked about the reasons for not having HZ vaccination,
approximately half (47.1%) replied that they were unaware of its
availability. This was followed by inadequate promotion from doctors and
public education (32.4%), the relatively high cost of the vaccine
(28.4%), and good self-perceived health (20.3%). Lastly, 17.2% replied
that they would consider HZ vaccination in the future.
Discussion
This study attempted to investigate the
knowledge, awareness, and attitudes towards HZ and its vaccination among
citizens aged 50 years or above in Hong Kong. The results were
informative. They revealed that the general public do not have adequate
knowledge about the diseases caused by VZV or awareness regarding the
prevention of HZ. This corroborates the general opinion of having an
inadequate understanding of the disease. Similar findings have been
observed in other countries according to a global survey,17
in which around 67% subjects stated they had little or no knowledge
about HZ.
Few respondents in this study knew that chickenpox (varicella zoster)
and shingles (HZ) are caused by the same virus. Similar results have
been reported by the Public Opinion Programme, the University of Hong Kong
(HKUPOP).5 Certain misconception about the disease
persists—death from a rash circumventing the body—is still a commonly
believed myth among the middle-aged and the elderly people. This study found
that the proportions of respondents who were aware of HZ and its
vaccination were comparable with those reported by a study in South
Korea.18
There was a significant association between educational attainment and
the correct responses regarding knowledge of HZ. The positive
correlation between a history of HZ and the number of correct
responses, however, was only marginally significant. There may be
several reasons. Physicians may not have given patients enough
information about the disease with consequent persistence of
misconceptions. Patients who have had the disease should not be presumed
to have a better understanding than those who have not. Moreover,
participants might be relatively less aware of HZ due to its less
life-interfering nature: only 35% were concerned about getting the
disease. Despite the relatively low perceived risk, approximately 77%
opined that HZ would have a significant effect on their health, whilst
66% admitted an interest in knowing more about the disease and its
prevention. Similar observations have been reported in other countries,17
where 26% predicted that they were likely to have HZ in the future, and
70% indicated that they would ask their doctors about HZ vaccination.
This study found that over 60% of respondents showed disagreement
regarding whether there was sufficient accessibility to information
about the prevention of HZ. This may contribute to a lack of awareness
of the HZ vaccine as the most common reason in our study for
non-vaccination. This serves to emphasise the substantial role of
doctors in health promotion regarding HZ in future.
According to the study conducted in South Korea,18
although 85.8% of participants would consider vaccination against HZ
initially, the figure fell to 59.6% when they took account of the
associated cost. On the contrary, HZ vaccination was considered by 17.2%
and 36.0% of respondents in this study and in the survey led by HKUPOP,5
respectively, suggesting that HZ vaccination is currently not widely
accepted by the community. The situations in Hong Kong and South Korea
are similar to some degree since participants expressed some interest in
vaccination but associated cost and recommendations from doctors were
key influences on a decision about whether or not to vaccinate.
Limitations
This study could be subject to selection bias
because participants were recruited via convenience sampling in one
clinic only. The results obtained from this study may have limited
generalisability to the GOPC setting and the general population. In
future studies, representative samples may be recruited from clinics in
various districts and specialties to achieve a more diverse group of
people and to further confirm the associations.
Several survey responses were invalidated. For instance, some people claimed that they had not had chickenpox before but had had HZ. This is biologically implausible and may be because most people got chickenpox as an infant or child.1 3 8 This hinders accurate recall unless family member can help. Recall bias is another recognised limitation of this study. Patients with a history of HZ or other chronic diseases usually pay greater attention to their health. Their medical history was subject to self-reported bias since such information could not be retrieved from their medical records.
Another source of bias comes from non-response. Those who refused to participate in the survey (13%) stated that they were unfamiliar with the disease. The results of this study may also be affected by responses that were speculative, as reflected by the observation that some respondents tended to guess rather than answer “uncertain or do not know”. These factors may overvalue the level of understanding of the disease among the general public that could have been improved by a pilot study to design questions with clear wordings and simple language. A pilot study would help identify respondents’ strategies in answering specific questions that required recall, to better evaluate their understanding of HZ, and establish the limits of recollection, with the effect of minimising bias, and enhancing accuracy and response completeness.
Further studies may be initiated to investigate the epidemiology of HZ in Hong Kong, and clarify whether there are significant associations of HZ knowledge with specific socio-demographic groups. Similar studies should also be conducted in younger adults.
Since 2014, the varicella zoster vaccine has been incorporated into the Hong Kong Childhood Immunisation Programme, under which children will be vaccinated against chickenpox at 1 year of age and during their first year of primary education.22 23 While this may offer protection against chickenpox and HZ for future generations, more studies are needed to determine whether it is also cost-effective to offer HZ vaccination to the population aged 50 years or above. This may have notable implications for its acceptance and practice.
Several survey responses were invalidated. For instance, some people claimed that they had not had chickenpox before but had had HZ. This is biologically implausible and may be because most people got chickenpox as an infant or child.1 3 8 This hinders accurate recall unless family member can help. Recall bias is another recognised limitation of this study. Patients with a history of HZ or other chronic diseases usually pay greater attention to their health. Their medical history was subject to self-reported bias since such information could not be retrieved from their medical records.
Another source of bias comes from non-response. Those who refused to participate in the survey (13%) stated that they were unfamiliar with the disease. The results of this study may also be affected by responses that were speculative, as reflected by the observation that some respondents tended to guess rather than answer “uncertain or do not know”. These factors may overvalue the level of understanding of the disease among the general public that could have been improved by a pilot study to design questions with clear wordings and simple language. A pilot study would help identify respondents’ strategies in answering specific questions that required recall, to better evaluate their understanding of HZ, and establish the limits of recollection, with the effect of minimising bias, and enhancing accuracy and response completeness.
Further studies may be initiated to investigate the epidemiology of HZ in Hong Kong, and clarify whether there are significant associations of HZ knowledge with specific socio-demographic groups. Similar studies should also be conducted in younger adults.
Since 2014, the varicella zoster vaccine has been incorporated into the Hong Kong Childhood Immunisation Programme, under which children will be vaccinated against chickenpox at 1 year of age and during their first year of primary education.22 23 While this may offer protection against chickenpox and HZ for future generations, more studies are needed to determine whether it is also cost-effective to offer HZ vaccination to the population aged 50 years or above. This may have notable implications for its acceptance and practice.
Conclusions
Hong Kong people generally have some knowledge
about the symptoms of HZ, and are aware that treatment is available for
active disease. Nonetheless, there remains unsatisfactory understanding
of the disease progression from chickenpox to HZ, and misconceptions
about the disease remain prevalent, particularly in the older age-group.
The lack of knowledge that HZ is preventable may be pertinent to the
relatively low awareness and acceptance of the HZ vaccine compared with
that for vaccines for other important diseases such as influenza and
pneumococcal pneumonia. Further public education about varicella zoster
and HZ, covering both disease features and effective prevention, will
help to empower health, rectify misconceptions, and reduce disease
burden in Hong Kong.
Acknowledgements
The authors would like to thank Dr Wendy WS Tsui
and Dr Alfred SK Kwong from the Department of Family Medicine and
Primary Health Care, Queen Mary Hospital, for their kind permission to
conduct the study in the Sai Ying Pun GOPC. We thank Dr LW Tian from the
Division of Epidemiology and Biostatistics, School of Public Health, the
University of Hong Kong, for his invaluable feedback and support. This
study was conducted by medical students as a Health Research Project
submitted to the School of Public Health, Li Ka Shing Faculty of
Medicine, the University of Hong Kong.
Declaration
All authors have disclosed no conflicts of interest.
References
1.Straus SE, Ostrove JM, Inchauspé G, et
al. NIH conference. Varicella-zoster virus infections. Biology, natural
history, treatment, and prevention. Ann Intern Med 1988;108:221-37. Crossref
2. Number of notifiable infectious
diseases by month in 2016. Centre for Health Protection, Department of
Health, Hong Kong SAR Government. Available from: http://www.chp.gov.hk/en/data/1/10/26/43/5128.html.
Accessed 11 May 2017.
3. Kangro HO, Osman HK, Lau YL, Heath RB,
Yeung CY, Ng MH. Seroprevalence of antibodies to human herpesviruses in
England and Hong Kong. J Med Virol 1994;43:91-6.
Crossref
4. Harpaz R, Ortega-Sanchez IR, Seward
JF, Advisory Committee on Immunization Practices (ACIP) Centers for
Disease Control and Prevention (CDC). Prevention of herpes zoster:
recommendations of the Advisory Committee on Immunization Practices
(ACIP). MMWR Recomm Rep 2008;57(RR-5):1-30.
5. Survey on herpes zoster vaccine.
Public Opinion Programme, The University of Hong Kong; 2013. Available
from: https://www.hkupop.hku.hk/english/report/prppl/index.html.
Accessed 29 Dec 2015.
6. Dworkin RH, Johnson RW, Breuer J, et
al. Recommendations for the management of herpes zoster. Clin Infect Dis
2007;44 Suppl 1:S1-26. Crossref
7. Gnann JW Jr, Whitley RJ. Clinical
practice. Herpes zoster. N Engl J Med 2002;347:340-6. Crossref
8. Joesoef RM, Harpaz R, Leung J, Bialek
SR. Chronic medical conditions as risk factors for herpes zoster. Mayo
Clin Proc 2012;87:961-7. Crossref
9. Sampathkumar P, Drage LA, Martin DP.
Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc
2009;84:274-80.
Crossref
10. Johnson RW, Wasner G, Saddier P,
Baron R. Postherpetic neuralgia: epidemiology, pathophysiology and
management. Expert Rev Neurother 2007;7:1581-95. Crossref
11. Panatto D, Bragazzi NL, Rizzitelli
E, et al. Evaluation of the economic burden of Herpes Zoster (HZ)
infection. Hum Vaccin Immunother 2015;11:245-62. Crossref
12. Yawn BP, Itzler RF, Wollan PC,
Pellissier JM, Sy LS, Saddier P. Health care utilization and cost burden
of herpes zoster in a community population. Mayo Clin Proc
2009;84:787-94. Crossref
13. Compendium of pharmaceutical
products 2015. Drug Office, Department of Health, Hong Kong SAR
Government; 2015.
14. FDA licenses new vaccine to reduce
older Americans’ risk of shingles. US Food and Drug Administration;
2006. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2006/ucm108659.htm.
Accessed 29 Dec 2015.
15. FDA approves Zostavax vaccine to
prevent shingles in individuals 50 to 59 years of age. US Food and Drug
Administration; 2011. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm248390.htm.
Accessed 29 Dec 2015.
16. Oxman MN, Levin MJ, Johnson GR, et
al. A vaccine to prevent herpes zoster and postherpetic neuralgia in
older adults. N Engl J Med 2005;352:2271-84.
Crossref
17. Paek E, Johnson R. Public awareness
and knowledge of herpes zoster: results of a global survey. Gerontology
2010;56:20-31. Crossref
18. Yang TU, Cheong HJ, Song JY, Noh JY,
Kim WJ. Survey on public awareness, attitudes, and barriers for herpes
zoster vaccination in South Korea. Hum Vaccin Immunother 2015;11:719-26.
Crossref
19. Faul F, Erdfelder E, Buchner A, Lang
AG. Statistical power analyses using G*Power 3.1: tests for correlation
and regression analyses. Behav Res Methods 2009;41:1149-60. Crossref
20. 2011 Population Census summary
results. Census and Statistics Department, Hong Kong SAR Government;
2012.
21. Elderly Vaccination Subsidy Scheme.
Centre for Health Protection, Department of Health, Hong Kong SAR
Government; 2015. Available from: http://www.chp.gov.hk/tc/view_content/21839.html.
Accessed 29 Dec 2015.