Hong Kong Med J 2017 Jun;23(3):264–71 | Epub 5 May 2017
DOI: 10.12809/hkmj166124
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
How well are we managing fragility hip fractures? A narrative report on the review with the attempt to set up a Fragility Fracture Registry in Hong Kong
KS Leung, MD, FHKCOS1;
WF Yuen, BNurs, MSc1;
WK Ngai, MB, BS, FHKCOS2;
CY Lam, MB, BS, FHKCOS3;
TW Lau, MB, BS, FHKCOS4;
KB Lee, MB, ChB, FHKCOS5;
KM Siu, MB, ChB, FHKCOS6;
N Tang, MB, ChB, FHKCOS7;
SH Wong, MB, BS, FHKCOS8;
WH Cheung, BSc, PhD1
1 Department of Orthopaedics and Traumatology, The Chinese University of Hong Kong, Shatin, Hong Kong
2 Department of Orthopaedics and Traumatology, North District Hospital,
Sheung Shui, Hong Kong
3 Department of Orthopaedics and Traumatology, Tuen Mun Hospital,
Tuen Mun, Hong Kong
4 Department of Orthopaedics and Traumatology, Queen Mary Hospital,
Pokfulam, Hong Kong
5 Department of Orthopaedics and Traumatology, Queen Elizabeth
Hospital, Jordan, Hong Kong
6 Department of Orthopaedics and Traumatology, Princess Margaret
Hospital, Laichikok, Hong Kong
7 Department of Orthopaedics and Traumatology, Prince of Wales
Hospital, Shatin, Hong Kong
8 Department of Orthopaedics and Traumatology, Caritas Medical Centre,
Shamshuipo, Hong Kong
Corresponding author: Dr KS Leung (ksleung@cuhk.edu.hk)
Abstract
Introduction: In setting up a disease registry for
fragility fractures in Hong Kong, we conducted a
retrospective systematic study on the management
of fragility hip fractures. Patient outcomes were
compared with the standards from our orthopaedic
working group and those from the British
Orthopaedic Association that runs a mature fracture
registry in the United Kingdom.
Methods: Clinical data on fragility hip fracture
patients admitted to six acute major hospitals in
Hong Kong in 2012 were captured. These included
demographics, pre- and post-operative assessments,
discharge details, complications, and 1-year follow-up
information. Analysis was performed according
to the local standards with reference to those from
the British Orthopaedic Association.
Results: Overall, 91.0% of patients received
orthopaedic care within 4 hours of admission
and 60.5% received surgery within 48 hours.
Preoperative geri-orthopaedic co-management
was received by 3.5% of patients and was one of the
reasons for the delayed surgery in 22% of patients.
Only 22.9% were discharged with medication that
would promote bone health. Institutionalisation on
discharge significantly increased by 16.2% (P<0.001).
Only 35.1% of patients attended out-patient follow-up
1 year following fracture, and mobility had
deteriorated in 69.9% compared with the premorbid
state. Death occurred in 17.3% of patients within a
year of surgery compared with 1.6% mortality rate in
a Hong Kong age-matched population.
Conclusions: The efficiency and quality of acute care
for fragility hip fracture patients was documented.
Regular geri-orthopaedic co-management can
enhance acute care. Much effort is needed to
improve functional recovery, prescription of bone
health medications, attendance for follow-up, and
to decrease institutionalisation. A Fracture Liaison
Service is vital to improve long-term care and
prevent secondary fractures.
New knowledge added by this study
- This was the first study to review the standards and clinical outcomes of 2914 patients from six major hospitals in Hong Kong with fragility hip fracture.
- Strengths and weaknesses of current fragility hip fracture management were identified. Recommendations are made to improve care.
- This study was the first phase in the process of setting up a Fragility Fracture Registry and reveals the usefulness of a disease registry for improving patient care.
Introduction
Fragility hip fracture is one of the most common
fragility fractures and is becoming one of the major
health care burdens on a society with an ageing
population. Statistics of the Hospital Authority (HA)
of Hong Kong (HK) reveal that the incidence of
fragility fractures in 2014 (14 000 cases) was much
higher than that for acute myocardial infarction
(6383 cases) or acute cerebrovascular accident
(11 187 cases). Number of patients admitted for hip
fracture surgery increased from 3678 in 2000 to 4579
in 2011, ie 24.5% in 11 years.1 Although the annual
age-specific risk of hip fracture slightly decreased, it is
estimated that with the projected ageing population,
fragility hip fractures in HK will number more than
6300 cases in 2020 and 14 500 cases in 2040, a 3-fold
increase from 2011.1 Approximately 30% of patients
under the age of 80 years were unable to walk
independently 1 year after hip fracture and became
home-bound; 20% to 40% of patients were admitted
to an elderly care home; and all patients suffered
both physically and psychologically with re-fracture
and fear of falls.2 Hip fracture patients with poor
functional recovery are unable to resume their pre-fracture
function with a consequent deterioration in
quality of life. Mortality at 1 year after hip fracture
was as high as 27% in males and 15% in females.1
To monitor the outcomes of management
and formulate standards of care in HK for fragility
hip fracture, the Coordinating Committee in
Orthopaedics & Traumatology of the HA proposed
a Fragility Fracture Registry (www.ffr.hk) in 2013.
It is hoped that the registry will ultimately help set
the standards of care with respect to local demands,
monitor patient care and implement preventive
measures, thus improving the cost-effectiveness of
fragility fracture care.
In the first phase of setting up the Fragility
Fracture Registry, a retrospective study was
conducted of fragility hip fractures treated at six
acute public hospitals under the management of the
HA. This study aimed to review the current fragility
hip fracture management in HK, and compare the
outcomes with the standards set by our working
group with reference to the six evidence-based
standards set by the British Orthopaedic Association
(BOA) for the care of patients with fragility hip
fracture.3
Methods
All patients with fragility hip fracture and admitted
in the calendar year 2012 to the six hospitals in
HK—Caritas Medical Centre, Prince of Wales
Hospital, Princess Margaret Hospital, Queen
Elizabeth Hospital, Queen Mary Hospital, and
Tuen Mun Hospital—which are located in different
clusters were included. Residents of HK aged 50
years and above with hip fracture sustained by a fall
from a standing height were recruited. The number
of fragility hip fractures from the six hospitals was
approximately 60% of the total fragility hip fractures
treated in Hong Kong during 2012. Those with
atypical or pathological fracture were excluded.
As 98% of patients with fragility hip fracture were
managed in public hospitals, eligible patients were
identified using the HA Clinical Data Analysis and
Reporting System with disease coding of acute hip
fracture (ICD-9-CM 820.X).4 Ethical approvals were obtained from all the six hospitals and the study was done in accordance with the principles outlined in the Declaration of Helsinki.
With reference to the National Hip Fracture
Database of the United Kingdom (UK NHFD)
and Scottish Hip Fracture Audit, the dataset was
designed according to the acute, rehabilitation, and
post-discharge practices in HK. Information was
derived from the HA Clinical Management System
and hospital records for the following: demographics,
preoperative and postoperative assessments,
surgical and discharge details, rehabilitation
details, out-patient follow-up consultations and
complications up to 1 year after fracture (Table 1).
All data were input and managed using the Research
Electronic Data Capture (REDCap) tool hosted at
the Department of Orthopaedics and Traumatology,
Faculty of Medicine, The Chinese University of Hong
Kong.5
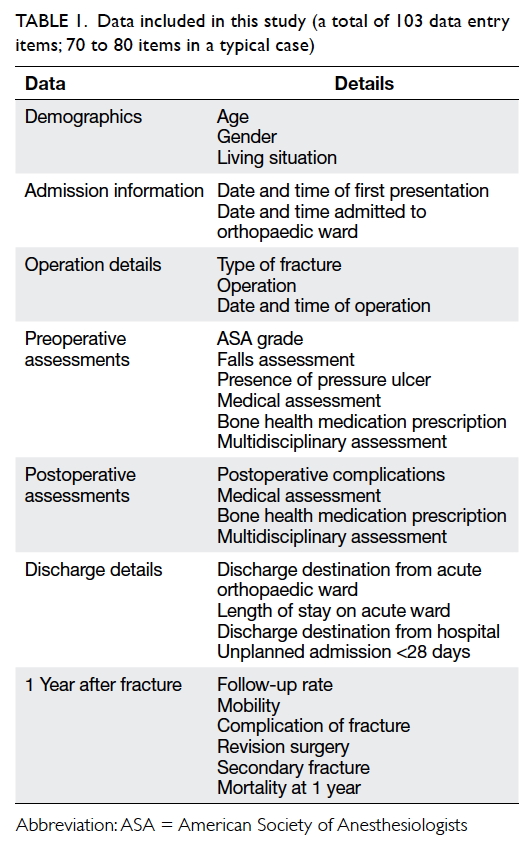
Table 1. Data included in this study (a total of 103 data entry items; 70 to 80 items in a typical case)
Data were input by research assistants who
understood medical terms and abbreviations. Data
were validated for one in five cases selected randomly
by six liaison teams located in the participating
hospitals and composed of orthopaedic surgeons
and nurses. Each liaison member was trained by the
central research team in data validation and REDCap
manipulation.
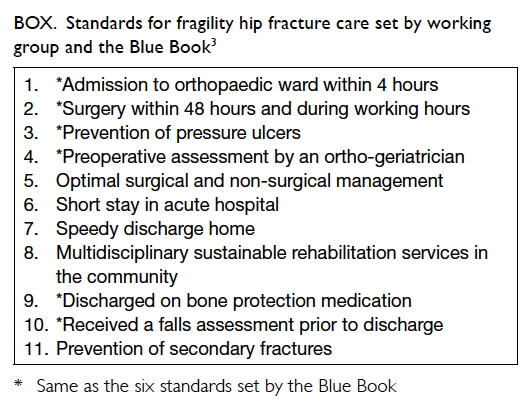
The data were analysed and compared with the
standards set by our working group with reference
to the six standards set by the BOA: Care of Patients
with Fragility Fractures (known as the Blue Book;
Box).3
Descriptive statistics were used to describe
the current hip fracture conditions in HK and
outcomes compared with standards of care from
HK orthopaedic working group with reference to
BOA. The percentage was calculated based on the
number of follow-up patients available at different
time-points. Chi squared test was used to compare
categorical data. The Statistical Package for the
Social Sciences (Windows version 20.0;
IBM Corp, Armonk [NY], US) was used to perform
statistical analysis. Significance was set at P<0.05.
Results
Demographics
A total of 2914 fragility hip fractures were captured
in the calendar year 2012 and the mean (± standard
deviation) patient age was 82.1 ± 8.6 years (range,
50-104 years). Of the patients, 1979 (67.9%) were
female; 2017 (73.7%) came from home and 719
(26.3%) from an elderly care home; 1119 (40.9%),
1541 (56.3%), and 20 (0.7%) patients had an American
Society of Anesthesiologists (ASA) score of grade 2,
3, and 4, respectively (Table 2).
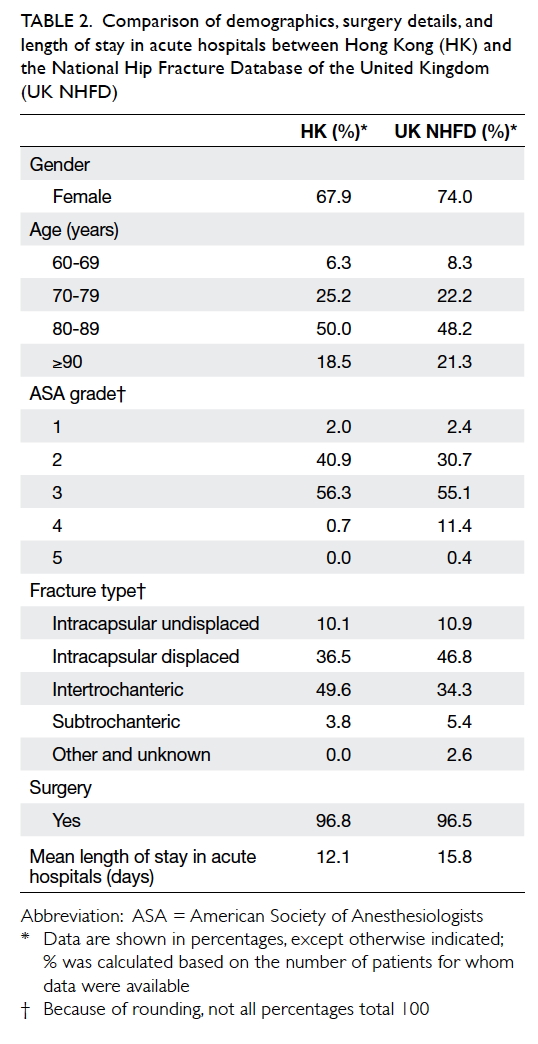
Table 2. Comparison of demographics, surgery details, and length of stay in acute hospitals between Hong Kong (HK) and the National Hip Fracture Database of the United Kingdom (UK NHFD)
Acute management
The mean time from presentation to the accident
and emergency department to orthopaedic care
was 2.3 hours (median time, 1.7 hours) with 91.0%
patients receiving orthopaedic care within 4 hours.
Geriatric or internal medicine review was performed
in 764 (27.8%) patients although only 95 (3.5%) were
routinely managed by a geriatrician preoperatively.
Surgery was performed in 2774 (96.8%)
patients. The mean time to surgery was 62.7 hours
(median time, 42.1 hours) with 1678 (60.5%)
undergoing surgery in exactly 48 hours and 2172
(78.3%) within 2 calendar working days.
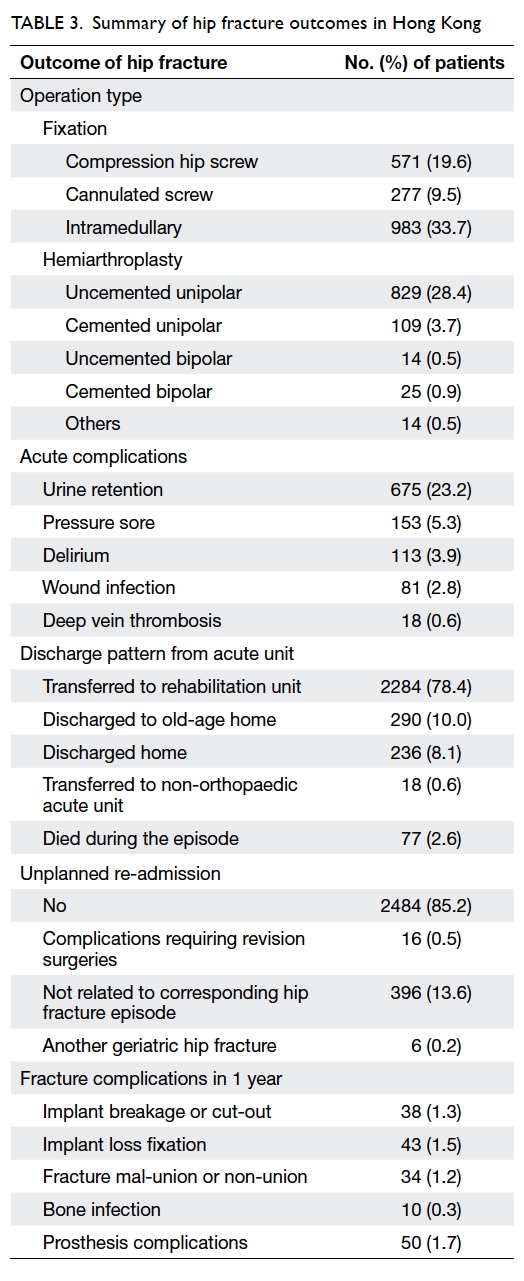
Intracapsular fracture occurred in 1358 (46.6%)
patients of whom 277 (9.5%) underwent cannulated
screw fixation, 829 (28.4%) uncemented unipolar
hemiarthroplasty, and 109 (3.7%) cemented unipolar
hemiarthroplasty. Intertrochanteric fracture
occurred in 1446 (49.6%) patients of whom 571
(19.6%) underwent compression hip screw fixation
and 983 (33.7%) intramedullary fixation (Tables 2 and 3).
During stay in acute hospitals, some of the
patients developed acute complications, with nearly
one fourth experienced urine retention. A small
number of patients developed other complications
like pressure sore, delirium, wound infection, and
deep vein thrombosis (Table 3).
The mean length of stay in acute hospitals was
12.1 days. With regard to the discharge destination
from the acute unit, a majority of patients (2284,
78.4%) were transferred to a rehabilitation unit,
290 (10.0%) to an old-age home, 236 (8.1%) to their
previous home, and 77 (2.6%) died during the acute
admission (Table 3).
Rehabilitation phase
Allied health professionals provided preoperative
multidisciplinary care to 1759 (64.0%) patients and
postoperative care to 2886 (99.4%). Bone health
medication was prescribed to 424 (15.3%) patients
preoperatively and 666 (22.9%) postoperatively.
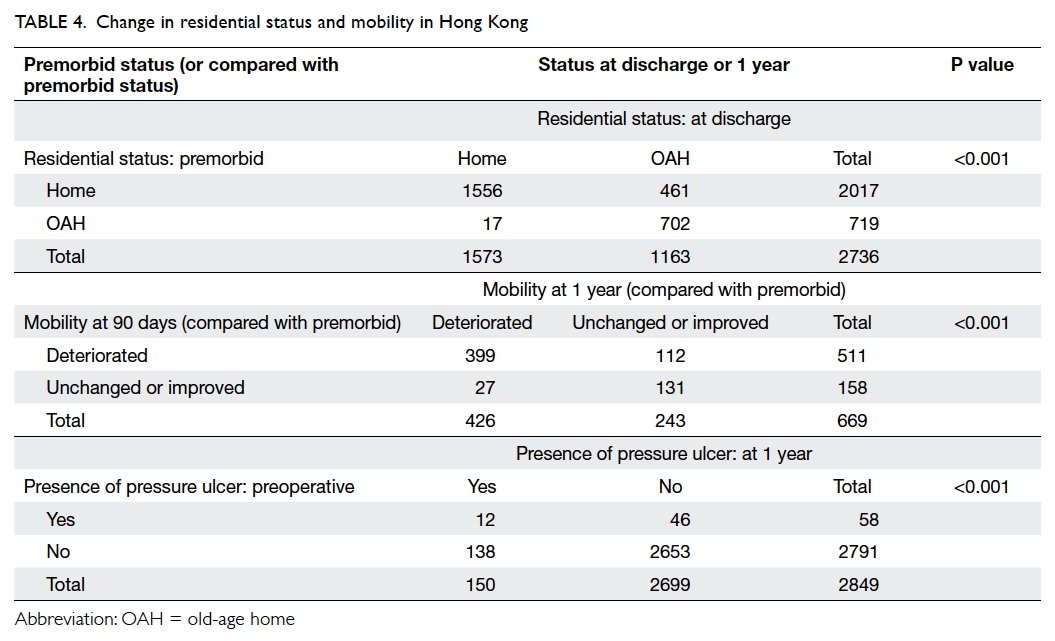
Just over half of all patients (n=1573, 57.5%) were
discharged to their home and 1163 (42.5%) to an
old-age home. Old-age home admission at discharge
significantly increased (P<0.001) [Table 4].
Post-discharge management
There was a declining trend over time for attendance
at follow-up; 2179 (74.8%) attended follow-up at 90
days after fracture, 2508 (86.1%) at 180 days, and
only 1023 (35.1%) at 1 year. Postoperative mobility
compared with premorbid had deteriorated at
90-day, 180-day, and 1-year follow-up in 1689
(77.5%), 2062 (82.2%), and 715 (69.9%) patients,
respectively. With those 669 patients available for
assessments at both 90-day and 1-year time-points,
511 patients had deterioration at 90 days and 426
patients deteriorated at 1 year. The deterioration was
significant at 1-year follow-up (P<0.001) [Table 4].
Pressure sores were evident or developed in 58 (2.0%)
patients preoperatively and 150 (5.3%) at 1 year.
Presence of pressure sore significantly increased at 1
year (P<0.001) [Table 4].
Fracture complications occurred in 175 (6.0%)
patients within a year (Table 3) with 90 (3.1%)
requiring revision surgery. A secondary fracture
occurred in 117 (4.0%) patients and 505 (17.3%)
patients died in 1 year compared with the 1.6%
mortality rate for a HK age-matched population.6 7
Discussion
This report reviewed the management of fragility
hip fractures in HK based on the standards of care
by our orthopaedic community and compared the
outcomes with the standards set by our working
group and by BOA in the UK.
The demographics were comparable to
previous studies in HK. The mean age of patients
with fragility hip fracture in our 2012 data was 82.1
years, unchanged compared with local data from
2000 to 2011.1 The female-to-male ratio was around
2:1 indicating an increase in male fragility hip
fractures compared with 2.5:1 from 2001 to 2010.4 8 This may be due to increasing life expectancy of
the HK male population9 and bone mineral density
(BMD) at the hip in men that decreases with age.10
There were 1257 (46.6%) femoral neck fractures,
1445 (49.6%) intertrochanteric fractures, and 110
(3.8%) subtrochanteric fractures, comparable with
a previous local study of 1342 hip fracture patients
from 2007 to 2010.8 The majority of patients had an
ASA score of 2 and 3, comprising 40.9% and 56.3%,
respectively and in line with Lau et al’s study.8 There
was a marked increase in hemiarthroplasties and
intramedullary fixations with 977 (33.5%) and 983
(3.7%) cases respectively in our study, compared
with Lau et al’s study that reported 362 (27%)
hemiarthroplasties and 218 (16%) cephalomedullary
nail fixations.8 This reflects a change in the surgical
treatment, possibly due to a lower re-operation
rate,11 better functional outcomes,12 and higher cost-effectiveness13 in patients treated with
hemiarthroplasty; and minimal rate of fixation
failure, less blood loss, and shorter length of hospital
stay in patients treated with intramedullary fixation.14
A low complication rate (6.0%) and revision
rate (3.1%) are testimony to the improved standard of
routine acute care, which includes early orthopaedic
care and early surgeries.
Consequences of fragility hip fracture
Poor functional recovery was evident in the large
proportion of patients (77.5%) with deteriorated
mobility at 90-day out-patient clinic follow-up, not
improved 1 year after fracture (69.9%). This compares
with less than half of treated patients who regained
their pre-fracture mobility in another study.15
According to an internal survey conducted at Prince
of Wales Hospital, only 22% of patients received
out-patient physiotherapy; the major reason (71%)
was “not referred”. Inadequate rehabilitation after
discharge may explain poor functional recovery after
hip fracture. On discharge, HK patients discharged to
an old-age home significantly increased from 26.3%
to 42.5%, ie a 16.2% increase in institutionalisation
compared with only 10.5% in a Spanish study.16
Poor functional recovery after hip fracture may
contribute to this high institutionalisation rate, as
fractures are significantly associated with mild-to-severe functional limitations.17 Lack of support
in the community may mean a lack of sustained
rehabilitation after discharge. Family support may
also be suboptimal as many elderly are alone at home
during the day.
Low follow-up attendance and high mortality
The attendance rate for out-patient clinic follow-up
was only 35.1% at 1 year. A high proportion of
elderly living alone (12.7% in 2011)18 and a high
institutionalisation rate (5.7% in 2014)19 may explain
the low follow-up rate due to lack of support.
The mortality at 1 year after fracture was 17.3%,
comparable with other local studies: 18.6% from
2000 to 20061 and 18.0% from 2001 to 2009,4 which are much higher than that for an age-matched
population (1.6%).6 7
Comparison with standards in the United Kingdom
Data from this review were also compared with those
of the UK NHFD 201220 collected from 180 hospitals
across the UK with patients managed according to
the UK Blue Book standards.3
Tables 2 and 5 summarise the demographics,
surgery details, length of stay in acute hospitals, and
comparison of six standards for hip fracture care
between HK and UK NHFD, respectively. Major
differences in hip fracture management between HK
and UK NHFD are identified.
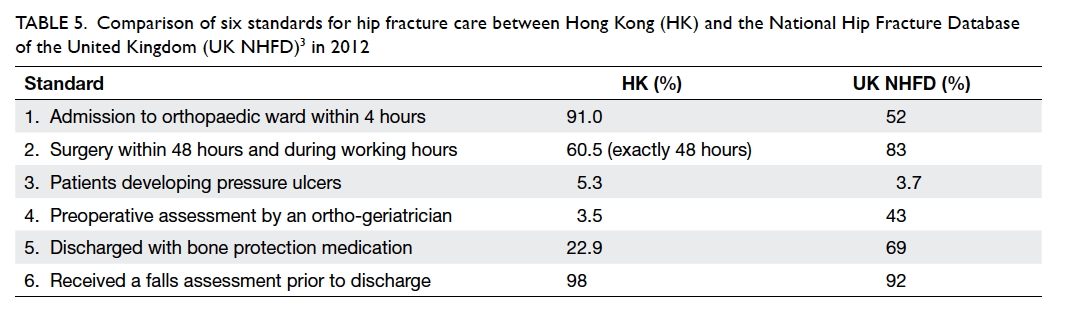
Table 5. Comparison of six standards for hip fracture care between Hong Kong (HK) and the National Hip Fracture Database of the United Kingdom (UK NHFD)3 in 2012
When comparing the demographics, our
review showed a larger male hip fracture population
(32%) than the UK (26%) while age and ASA grade
distribution were similar. Patients treated surgically
were similar in both databases; more HK patients
had intertrochanteric fracture (49.6% vs 34.3%)
and more UK patients had displaced intracapsular
fracture (46.8% vs 36.5%). The length of stay in acute
hospitals in HK was shorter than in UK (12.1 days vs
15.8 days). The mean length of post-acute stay in the
UK was only 4.4 days, however, which is shorter than
that in HK (around 3-4 weeks). This may be due to the
differences in acute and post-discharge care between
HK and the UK. Care by a general practitioner after
being discharged from hospital is the usual practice
in the UK; in HK, most patients will be cared for by
an orthopaedic team in post-acute rehabilitation
with follow-up in orthopaedic specialist clinics until
discharge.
In HK, 98% of patients underwent a falls
assessment on admission, similar to the UK (92%).
In HK, a Morse Fall Scale27 will be calculated by
orthopaedic nurses on admission; in the UK, a
systematic assessment is performed by a geriatrician
or a specialist nurse to prevent further falls.8
Quick surgery under Key Performance Indicator
With regard to the six standards for hip fracture care
set by the BOA Blue Book (Box and Table 5), 61%
of HK patients had surgery within exactly 48 hours,
compared with 35% in Spain21 and less than 10% in
China22; in the UK, 83% of patients received surgery
within 48 hours and during working hours. The
percentage of HK patients who underwent surgery
within 2 calendar working days was 30% before 2007 and
improved to 62% in 2008 after the establishment
of Key Performance Indicator (KPI) by the HA and
78.3% in 2012.23 The aim of KPI is to ensure 70% of hip
fracture patients receive surgery within 2 calendar working
days.24 25 This may explain why a large proportion of patients had quick hip fracture surgery in HK. The
delay in surgery for 22% of patients may have been
due to time spent awaiting medical optimisation by
physicians or geriatricians.
Importance of geri-orthopaedic co-management
Very few patients in HK (3.5%) received preoperative
assessment by geriatricians in contrast to 43% of
patients in the UK. In this review, only one of the
six studied hospitals had a geriatrician who routinely
assessed hip fracture patients pre- and post-operatively,
indicating a lack of geri-orthopaedic
co-management in HK. Studies have shown better
outcomes after hip fracture when patients receive
geri-orthopaedic treatment, with a lower 1-year
mortality rate,26 27 reduced acute hospital stay, and less need for further rehabilitation.27 A local study
reviewed the effectiveness of geri-orthopaedic co-management
and found that in the geri-orthopaedic
group, time to surgery was shorter, 1-year mortality
rate was lower, and more remained independent in
daily living activities.28 Therefore, geri-orthopaedic
care should be implemented in all hospitals in HK to
achieve better patient care. This will further improve
the KPI for fragility hip fractures in all hospitals in
HK.
Low prescription rate of bone protection medication
Only 23% of HK patients were discharged with
bone protection medication compared with almost
70% in the UK (Table 5) and nearly 40% in Korea
(excluding calcium and vitamin D).29 A local study
showed that 33% were prescribed medications for
osteoporosis in the 6 months after discharge.30
Osteoporosis diagnosis and treatment were driven
by BMD measurement, not fracture history.30
This may explain the low prescription rate of bone
protection medication when the fracture patient
did not undergo BMD measurement for a variety of
reasons such as unavailability of dual-energy X-ray
absorptiometry (DXA), long queuing time, or lack
of referral from orthopaedic doctors. Although the
need for DXA measurement prior to prescription
of bone health medication to patients with fragility
fracture remains controversial, it is clear that DXA
measurement is not the only single indication for
such medication.31
Importance of Fracture Liaison Services
In view of the low follow-up rate, poor functional
recovery, increased institutionalisation, and high
mortality after fragility hip fracture, better post-discharge
rehabilitation and secondary fracture
prevention should be implemented to restore
patients’ physical and psychological status.
Fracture Liaison Services (FLS) is a coordinator-based
service for sustained rehabilitation in the
community and secondary fracture prevention
in patients with fragility fractures. It has been
implemented in many countries—eg the UK,32
Australia,33 Canada34—and studies reveal that
FLS is cost-effective. Implementation of FLS in
HK may improve current post-discharge care.
Such services include osteoporosis identification
and treatment (eg DXA scan and prescription of
bone protection medication), education about
secondary fracture prevention (exercise, dietary
guidelines, and an education programme), and
sustainable multidisciplinary services (follow-up by
FLS coordinator regularly). With FLS, fragility hip
fracture patients with osteoporosis can be identified
and treated promptly with good compliance with
medications. Patients will be instructed to exercise
to improve functional status with a potential
consequent decrease in old-age home admission.
They will also be taught about falls prevention and
sustained rehabilitation, and hence lower the chance
of secondary fracture.
Limitations of this study
This study included approximately 60% of all
HK fragility hip fractures. It would be better to
include all HK hospitals in future studies to reflect
the full situation across the territory. This study
retrospectively reviewed medical records from 2012
with data retrieved from electronic and handwritten
records so a small percentage of data may have been
missing due to illegible records. A standardised
electronic format from the Clinical Management
System will improve data capture and analysis.
A disease registry is important to enable better
documentation.
Conclusions
This study reviewed the current fragility hip fracture
care in HK. Although acute surgical treatment
complies with international standards, standardised
geri-orthopaedic co-management will further
improve the acute care. Recognising fragility hip
fracture as a chronic disease model, the increased
rate in old-age home admission, poor functional
recovery, low prescription rate of bone health
medications, and low attendance rate for follow-up
were identified as problems in subsequent
management. These may explain the higher 1-year
mortality rate, high secondary fracture rate, and
deterioration in the quality of life after fracture
among these elderly. With an ageing population
and increasing longevity, the hip fracture rate is
expected to increase continuously. A comprehensive
multidisciplinary chronic disease management model
that includes geri-orthopaedic co-management and
FLS programmes should be implemented to improve
patient outcomes, prevent secondary fractures, and
reduce the economic burden on HK. The setting up
and maintenance of a registry of all fragility fractures
is imminent and will help health care professionals
monitor and continuously improve the standards of
patient care as well as prevent fractures.
Acknowledgements
This study was partially supported by grant support
of Asian Association for Dynamic Osteosynthesis
(Ref: AADO-RF2012-001-2Y) and Professional
Services Development Assistance Scheme,
Commerce and Economic Development Bureau,
Government of the Hong Kong Special Administrative Region. The authors would like to thank the liaison
teams that comprised doctors and nurses of the
Department of Orthopaedics and Traumatology
from the six participating hospitals for their help in
data validation.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Man LP, Ho AW, Wong SH. Excess mortality for operated
geriatric hip fracture in Hong Kong. Hong Kong Med J
2016;22:6-10. Crossref
2. Fierens J, Broos PL. Quality of life after hip fracture surgery
in the elderly. Acta Chir Belg 2006;106:393-6. Crossref
3. The care of patients with fragility fracture. British
Orthopaedic Association; 2007.
4. Chau PH, Wong M, Lee A, Ling M, Woo J. Trends in hip
fracture incidence and mortality in Chinese population
from Hong Kong 2001-09. Age Ageing 2013;42:229-33. Crossref
5. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N,
Conde JG. Research electronic data capture (REDCap)—a
metadata-driven methodology and workflow process for
providing translational research informatics support. J
Biomed Inform 2009;42:377-81. Crossref
6. Population estimates. Census and Statistics Department,
Hong Kong SAR Government; 2016.
7. Tables on health status and health services 2012.
Department of Health, Hong Kong SAR Government;
2013.
8. Lau TW, Fang C, Leung F. The effectiveness of a geriatric
hip fracture clinical pathway in reducing hospital and
rehabilitation length of stay and improving short-term
mortality rates. Geriatr Orthop Surg Rehabil 2013;4:3-9. Crossref
9. Women and men in Hong Kong key statistics. Census and
Statistics Department, Hong Kong SAR Government; 2016.
10. Lau EM, Leung PC, Kwok T, et al. The determinants of
bone mineral density in Chinese men—results from Mr.
Os (Hong Kong), the first cohort study on osteoporosis in
Asian men. Osteoporos Int 2006;17:297-303. Crossref
11. Shields E, Kates SL. Revision rates and cumulative financial
burden in patients treated with hemiarthroplasty compared
to cannulated screws after femoral neck fractures. Arch
Orthop Trauma Surg 2014;134:1667-71. Crossref
12. Gjertsen JE, Vinje T, Engesaeter LB, et al. Internal screw
fixation compared with bipolar hemiarthroplasty for
treatment of displaced femoral neck fractures in elderly
patients. J Bone Joint Surg Am 2010;92:619-28. Crossref
13. Waaler Bjornelv GM, Frihagen F, Madsen JE, Nordsletten
L, Aas E. Hemiarthroplasty compared to internal fixation
with percutaneous cannulated screws as treatment of
displaced femoral neck fractures in the elderly: cost-utility
analysis performed alongside a randomized, controlled
trial. Osteoporos Int 2012;23:1711-9. Crossref
14. Ma KL, Wang X, Luan FJ, et al. Proximal femoral nails
antirotation, Gamma nails, and dynamic hip screws for
fixation of intertrochanteric fractures of femur: a meta-analysis.
Orthop Traumatol Surg Res 2014;100:859-66. Crossref
15. Vochteloo AJ, Moerman S, Tuinebreijer WE, et al. More
than half of hip fracture patients do not regain mobility
in the first postoperative year. Geriatr Gerontol Int
2013;13:334-41. Crossref
16. Uriz-Otano F, Pla-Vidal J, Tiberio-López G, Malafarina
V. Factors associated to institutionalization and mortality
over three years, in elderly people with a hip fracture—An
observational study. Maturitas 2016;89:9-15. Crossref
17. Woo J, Ho SC, Yu LM, Lau J, Yuen YK. Impact of chronic
diseases on functional limitations in elderly Chinese aged
70 years and over: a cross-sectional and longitudinal
survey. J Gerontol A Bio Sci Med Sci 1998;53:M102-6. Crossref
18. Thematic report: older persons. Census and Statistics
Department, Hong Kong SAR Government; 2011.
19. Challenges of population ageing. Research Brief, Issue
1, 2015-2016. Hong Kong: Research Office, Legislative
Council Secretariat; 2015.
20. National report 2012. The UK National Hip Fracture
Database; 2012.
21. Vidán MT, Sánchez E, Gracia Y, Marañón E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients
with hip fracture: a cohort study. Ann Intern Med 2011;155:226-33. Crossref
22. Tian M, Gong X, Rath S, et al. Management of hip fractures
in older people in Beijing: a retrospective audit and
comparison with evidence-based guidelines and practice
in the UK. Osteoporos Int 2016;27:677-81. Crossref
23. Lau PY. To improve the quality of life in elderly people.
Hong Kong Med J 2016;22:4-5.
24. New framework for key performance indicators (AOM-P530).
Hong Kong: Hospital Authority; 2008.
25. Guidebook on key performance indicators. 2nd ed. Hong
Kong: Hospital Authority; 2015.
26. Folbert EC, Hegeman JH, Vermeer M, et al. Improved
1-year mortality in elderly patients with a hip fracture
following integrated orthogeriatric treatment. Osteoporos
Int 2017;28:269-77. Crossref
27. Henderson CY, Shanahan E, Butler A, et al. Dedicated
orthogeriatric service reduces hip fracture mortality. Ir J
Med Sci 2017;186:179-84. Crossref
28. Leung AH, Lam TP, Cheung WH, et al. An orthogeriatric
collaborative intervention program for fragility fractures: a
retrospective cohort study. J Trauma 2011;71:1390-4. Crossref
29. Kim SC, Kim MS, Sanfélix-Gimeno G, et al. Use of
osteoporosis medications after hospitalization for hip
fracture: a cross-national study. Am J Med 2015;128:519-26.e1. Crossref
30. Kung AW, Fan T, Xu L, et al. Factors influencing diagnosis
and treatment of osteoporosis after a fragility fracture
among postmenopausal women in Asian countries: a
retrospective study. BMC Womens Health 2013;13:7. Crossref
31. Ito K, Leslie WD. Cost-effectiveness of fracture prevention
in rural women with limited access to dual-energy X-ray
absorptiometry. Osteoporos Int 2015;26:2111-9. Crossref
32. McLellan AR, Gallacher SJ, Fraser M, McQuillian C.
The fracture liaison service: success of a program for the
evaluation and management of patients with osteoporotic
fracture. Osteoporos Int 2003;14:1028-34. Crossref
33. Cooper MS, Palmer AJ, Seibel MJ. Cost-effectiveness of
the Concord Minimal Trauma Fracture Liaison service,
a prospective, controlled fracture prevention study.
Osteoporos Int 2012;23:97-107. Crossref
34. Bogoch ER, Elliot-Gibson V, Beaton DE, Jamal SA, Josse
RG, Murray TM. Effective initiation of osteoporosis
diagnosis and treatment for patients with a fragility
fracture in an orthopaedic environment. J Bone Joint Surg
Am 2006;88:25-34. Crossref