Hong Kong Med J 2017 Apr;23(2):122–8 | Epub 12 Dec 2016
DOI: 10.12809/hkmj164872
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Management of traumatic patellar dislocation in
a regional hospital in Hong Kong
HL Lee, FHKCOS, FHKAM (Orthopaedic Surgery);
WP Yau, FHKCOS, FHKAM (Orthopaedic Surgery)
Division of Sports and Arthroscopic Surgery, Department of Orthopaedics
and Traumatology, Queen Mary Hospital, Hong Kong
This paper was presented at the Hong Kong Orthopaedic Association 35th
Annual Congress, 7 November 2015, Hong Kong.
Corresponding author: Dr HL Lee (ricklhl@gmail.com)
A video clip showing management of traumatic patellar dislocation is available at www.hkmj.org
Abstract
Introduction: The role of surgery for acute patellar
dislocation without osteochondral fracture is
controversial. The aim of this study was to report
the short-term results of management of patellar
dislocation in our institute.
Methods: Patients who were seen in our institution
with patella dislocation from January 2011 to April
2014 were managed according to a standardised
management algorithm. Pretreatment and 1-year
post-treatment International Knee Documentation
Committee score, Tegner activity level scale score,
and presence of apprehension sign were analysed.
Results: A total of 41 patients were studied of whom
20 were first-time dislocators and 21 were recurrent
dislocators. Among the first-time dislocators, there
was a significant difference between patients who
received conservative treatment versus surgical
management. The conservative treatment group
had a 33% recurrent dislocation rate, whereas there
were no recurrent dislocations in the surgery group.
There was no difference in Tegner activity level scale
score or apprehension sign before and 1 year after
treatment, however. Among the recurrent dislocators,
there was a significant difference between those who
received conservative treatment and those who
underwent surgery. The recurrent dislocation rate
was 71% in the conservative treatment group versus
0% in the surgery group. There was also significant
improvement in International Knee Documentation
Committee score from 67.7 to 80.0 (P=0.02), and of
apprehension sign from 62% to 0% (P<0.01).
Conclusions: A management algorithm for patellar
dislocation is described. Surgery is preferable
to conservative treatment in patients who have
recurrent patellar dislocation, and may also be
preferable for those who have an acute dislocation.
New knowledge added by this study
- This study reveals the short-term results regarding local management of traumatic patellar dislocation. A suggested treatment algorithm is provided that can help approach this problem systematically.
- The results of this study support surgery as the first-line treatment of recurrent patellar dislocation. It is inconclusive whether conservative treatment or surgery is preferable in first-time dislocators although there is a trend towards better results with surgery.
Introduction
Patellar dislocation is a common injury in young,
active individuals and accounts for approximately
3% of all knee injuries. The overall incidence is about
1 in 1000.1 2 Without appropriate treatment, these
injuries may result in significant morbidity, including
significant limitations in activity and patellofemoral
arthritis.3 4 The management of patellar dislocation must take into account numerous clinical factors
including the number of dislocations, chronicity of
the dislocation, bony alignment, and status of the
articular cartilage.
The management of acute first-time patellar
dislocators is controversial. Traditionally, these
patients have been managed conservatively but
the results of such treatment are highly variable
and unpredictable. The recurrent instability rate
following conservative treatment in these patients
has been reported to be between 17% and 44%.1 5
Limitation of strenuous activity after conservative
treatment was reported in 58% of these patients, and
failure to return to sports activity in 55%.4 Therefore
some authors have recommended early primary
surgical stabilisation for this group of patients.3 6 7
Surgery is also indicated in patients who have
concomitant osteochondral fractures.8
The management of recurrent patellar
dislocators is less controversial. Studies have shown
that in patients who have had two dislocations, the
risk of further dislocation is as high as 50%.1 Most
surgeons would recommend surgical stabilisation
for these patients.
The aim of this study was to review and
document the short-term results of management of
patients with traumatic patellar dislocations in our
institute, which is a university hospital that serves
as a tertiary and quaternary referral centre in Hong
Kong.
Methods
Patients with patellar dislocation who were seen in
our institution from January 2011 to April 2014 were
included in the current study. All patients were cared
for according to the institution’s patellar dislocation
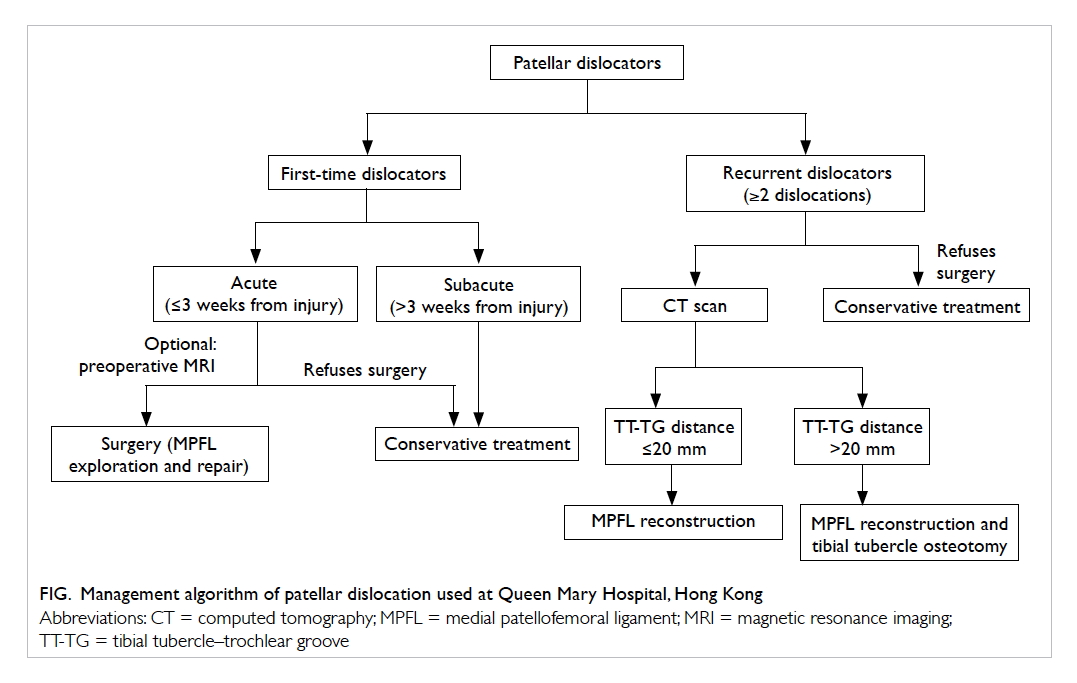
management algorithm (Fig).
Patients followed up for less than 1 year were
excluded from the study. Those who had chronic
dislocations (persistent dislocation for more than 6
weeks’ duration) and a history of patellar
surgery or osteochondral fracture detected on X-ray
were also excluded.
The patellar dislocation management
algorithm used in our institution is as follows.
Patients are first categorised as first-time dislocators
or recurrent dislocators. First-time dislocators are
further subcategorised as an acute dislocator or
subacute dislocator according to the time interval
between presentation and time of injury. If this
time interval is 3 weeks or less, they are considered
acute dislocators; if more than 3 weeks, they are
subcategorised as subacute dislocators.
For first-time acute dislocators, medial
patellofemoral ligament (MPFL) repair surgery is
advised. Preoperative magnetic resonance imaging
(MRI) is not routinely performed. The exact site
of MPFL tear is identified intra-operatively by
combining knee arthroscopy and MPFL endoscopy.
If the MPFL is found avulsed at the femoral origin
or patellar insertion, it is repaired to bone using
suture anchors. If the MPFL is torn at mid-substance,
a direct end-to-end repair is performed. Minimal
plication of the medial retinaculum was observed in
all our cases. A hinged knee brace from full extension
to 20-degree flexion is applied for 3 weeks, followed
by patellar stabilisation orthosis for another 3 weeks.
Supervised physiotherapy in terms of quadriceps
strengthening exercises, range of motion training,
and patellar mobilisation exercises is offered for 3
to 6 months and the patient is also advised to avoid
pivoting sports for at least 6 months.
For first-time subacute dislocators,
conservative treatment is offered. This includes
wearing of a patellar stabilisation orthosis for a
total of 6 weeks after the dislocation and a period
of supervised physiotherapy (focusing on quadriceps
strengthening exercises and range of motion training)
for at least 6 weeks to 3 months. Patients are advised
to avoid any pivoting sports for a total of 6 months.
A similar regimen of conservative treatment is
offered to those first-time acute dislocators who
refuse surgical intervention. The whole course of
rehabilitation usually lasts 4 to 6 months before the
patient is permitted to resume full activity.
For recurrent dislocators, patients are advised
to have MPFL reconstruction. Plain computed
tomography of the knee is performed to measure
the tibial tubercle–trochlear groove (TT-TG)
distance. If this distance measures ≤20 mm, MPFL
reconstruction surgery is advised. If this distance
measures >20 mm, MPFL reconstruction and tibial
tubercle osteotomy surgery for anteromedialisation
of the tibial tubercle are advised. The rehabilitation
protocol following MPFL reconstruction is the same
as that for MPFL repair. For recurrent dislocators
who refuse surgery, conservative treatment is
advised. This consists of a 3- to 6-month course of
supervised physiotherapy.
The following outcome measures were
recorded before treatment and 1 year after
treatment in our study patients: (1) International
Knee Documentation Committee (IKDC) score; (2)
Tegner activity level scale score; and (3) presence
of apprehension sign on physical examination. The
redislocation rate at 1 year after treatment was also
measured for the different groups of treatment.
The IKDC score is a knee-specific self-evaluation
score for reporting patient symptoms,
function, and sports activity.9 Tegner activity level
scale score is a functional score describing a patient’s
activity level.10 The presence of apprehension sign
was documented by one of the two observers, who
were experienced sports surgeons in the authors’
institute. The test was performed with the patient
lying supine on the examination couch. The knee was
passively flexed to 20 degrees. A lateral displacing
force was applied manually on the medial side of
patella in an attempt to sublux the patella laterally.
Apprehension sign was defined as positive if the
patient reported a sense of subluxation or attempted
to stop the examiner.
Data were analysed and compared with the
Statistical Package for the Social Sciences (Windows
version 23.0; SPSS Inc, Chicago [IL], US). The
Wilcoxon signed-rank test (non-parametric, paired
samples test) was used to compare IKDC score and
Tegner activity level scale results before and
after treatment within the same treatment group. The
McNemar test (non-parametric, paired samples test)
was used to compare the percentage of patients with
apprehension sign before and after treatment within
the same treatment group. The Mann-Whitney U
test (non-parametric, independent samples test)
was used to compare IKDC score as well as Tegner
activity level scale results between conservative
treatment group and surgery group. The Pearson’s
Chi squared test (non-parametric, independent
samples test) was used to compare the percentage of
patients with apprehension sign as well as recurrent
dislocation rate between conservative treatment
group and surgery group. Whenever expected
counts were less than five, Fisher’s exact test was
used instead of Pearson’s Chi squared test. This study was done in accordance with the principles outlined in the Declaration of Helsinki.
Results
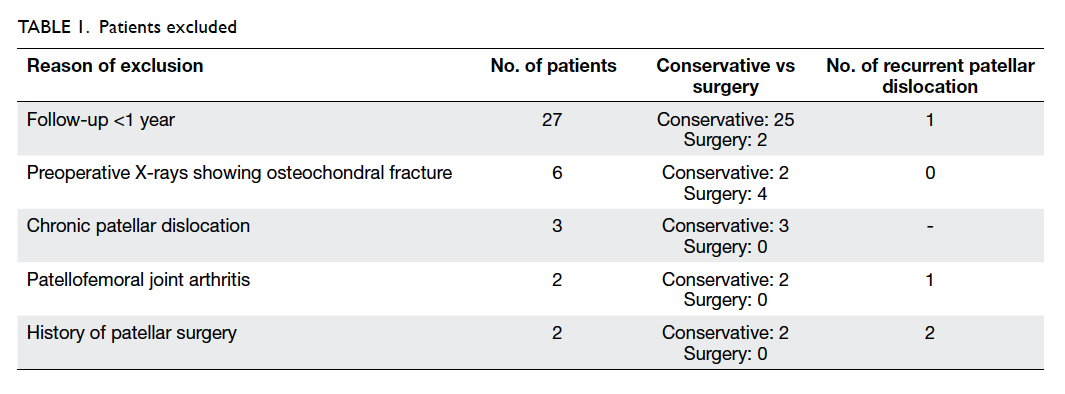
A total of 81 patients were identified. Of these,
40 patients were excluded—27 were excluded
due to follow-up of less than 1 year, six due to
osteochondral injury detected by X-ray, three due
to chronic dislocation, two due to development
of patellofemoral osteoarthritis, and two due to a
history of patellar surgery (Table 1). This
left us with 41 patients comprising 17 males and 24
females. Their mean age was 23.6 years (range, 13-44;
standard deviation, 7.4 years). A summary of
patient demographics is shown in Table 2.
There were 20 patients who were first-time
dislocators and 21 patients who were recurrent
dislocators. Among the first-time dislocators
(n=20), 45% (n=9) were treated conservatively and
55% (n=11) were treated with MPFL repair surgery.
Among the recurrent dislocators, 33% (n=7) were
treated conservatively, 62% (n=13) were treated with
MPFL reconstruction surgery, and 5% (n=1) were
treated with combined tibial tubercle osteotomy
and MPFL reconstruction surgery. Their results are
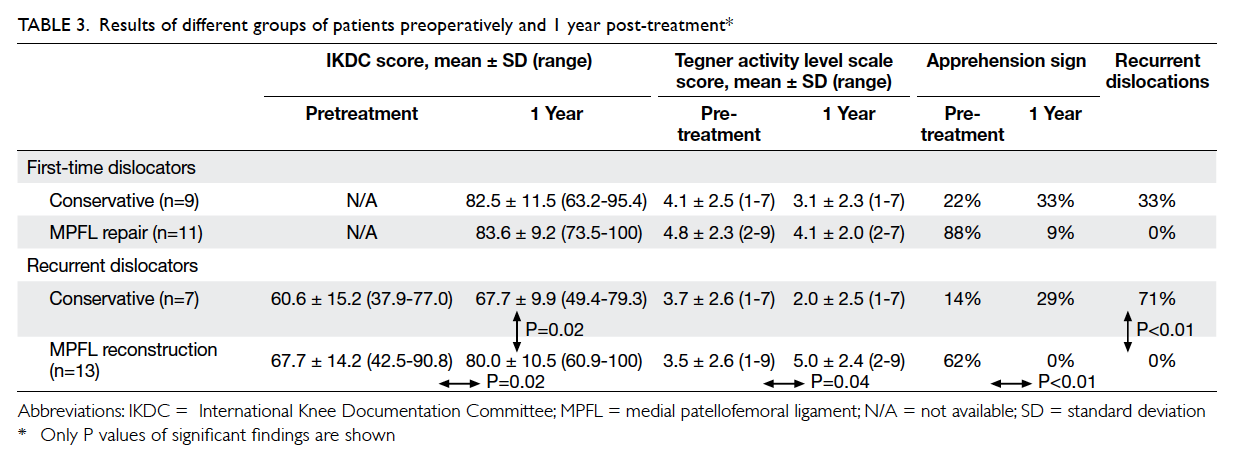
summarised in Table 3.
Among the first-time dislocators who received
conservative treatment (n=9), recurrent dislocation
occurred in 33% (n=3) within 1 year of treatment.
The findings are shown in Table 3. There were no
statistically significant differences between the
Tegner activity level scale or percentage of patients
with apprehension sign before and 1 year after
treatment.
Among the first-time dislocators who
underwent MPFL repair surgery (n=11), intra-operative
MPFL exploration showed 55% (n=6) of
them had tears at the patellar insertion, 27% (n=3)
had MPFL tear at the femoral origin, and 18% (n=2)
had MPFL mid-substance tear (one of which was
only a partial mid-substance tear). Preoperative
MRI was performed in seven of the 11 patients.
Among six of these seven patients, MPFL detected
on preoperative MRI correlated with the tear site on
intra-operative MPFL exploration. In the remaining
patient, only a partial tear of MPFL at mid-substance
was found intra-operatively; this was not detected
by the preoperative MRI. Regarding the outcome of
surgery, there were no recurrent dislocations within
1 year of surgery (Table 3). Apprehension sign was
present in 88% before surgery and 9% 1 year after
surgery (P=0.07, McNemar test). There were no
statistically significant differences between the
Tegner activity level scale or percentage of patients
with apprehension sign before and 1 year after
surgery.
Comparison of first-time dislocators who
received conservative treatment with first-time
dislocators who underwent MPFL repair surgery 1
year after treatment revealed no significant difference
in IKDC score. There was a lower percentage of
patients with apprehension sign (9% vs 33%) and
a lower rate of redislocation in the MPFL repair
surgery group (0% vs 33%, P=0.07, Fisher’s exact test)
but the differences were not statistically significant.
Among the recurrent dislocators who received
conservative treatment (n=7), recurrent dislocation
occurred in 71% (n=5) of patients within 1 year of
treatment (Table 3). Apprehension sign was present
in 14% before treatment and 29% 1 year after
treatment. There was no statistically significant
difference between the IKDC score, Tegner
activity level scale, or percentage of patients with
apprehension sign before and 1 year after treatment.
Among the recurrent dislocators who
underwent MPFL reconstruction surgery (n=13),
there were no recurrent dislocations within 1
year of surgery (Table 3). Apprehension sign was
present in 62% before surgery and no patients had
apprehension sign 1 year after surgery. There were
statistically significant improvements in the IKDC
score (P=0.02, Wilcoxon signed-rank test), Tegner
activity level scale score (P=0.04, Wilcoxon signed-rank
test), as well as percentage of patients with
apprehension sign (P<0.01, McNemar test).
One year after treatment, comparison of
recurrent dislocators who received conservative
treatment with recurrent dislocators who underwent
MPFL reconstruction surgery revealed that the
mean IKDC score was significantly better in the MPFL
reconstruction surgery group (80.0 vs 67.7; P=0.02,
Mann-Whitney U test). The redislocation rate was
significantly lower in the MPFL reconstruction
surgery group (0% vs 71%; P<0.01, Fisher’s exact
test). There was a lower percentage of patients with
apprehension sign in the MPFL reconstruction
surgery group (0% vs 29%) although the difference
was not statistically significant.
Discussion
For acute first-time patellar dislocators, it has been
widely agreed that in the presence of concomitant
osteochondral fracture, surgical treatment is
indicated.11 The indication of surgery for acute first-time
patellar dislocators without osteochondral
fractures is controversial. The recurrent instability
rate after conservative treatment in these patients has
been reported to be 17% to 44%.1 5 It has traditionally been held that these patients should be treated
conservatively.11 Nine prospective randomised
controlled trials have compared conservative and
surgical treatment in first-time dislocators and the
results have been inconsistent.12 13 14 15 16 17 18 19 20 In their systematic
review, Stefancin and Parker11 recommended
conservative treatment for most patients after first-time
dislocation, except those with concomitant
osteochondral fracture and those with significant
medial soft tissue damage who may benefit more
from surgical treatment. Smith et al21 reviewed 11
studies that included five randomised controlled
trials. They found that surgical treatment of patellar
dislocation was associated with a significantly
higher risk of patellofemoral joint osteoarthritis
but a significantly lower risk of subsequent patellar
dislocation compared with conservative treatment.21
A recent Cochrane review of six studies with 344
participants found that participants managed
surgically had a significantly lower risk of recurrent
dislocation following first-time dislocation at 2 to 9
years of follow-up compared with those managed
conservatively.22 There were no differences in physical
function scores. The authors, however, pointed out
that the quality of evidence was very low because of
the high risk of bias and the imprecision of the effect
estimates.22 They recommended that adequately
powered, multicentre, randomised controlled trials
are needed to substantiate this evidence.22 Erickson
et al23 carried out a systematic review of four meta-analyses
on surgical treatment of first-time patellar
dislocations. Three meta-analyses showed a lower
subsequent patellar dislocation rate in first-time
dislocators managed surgically compared with those
managed conservatively, whereas one meta-analysis
did not show any difference in redislocation rates.
Using the combined results of all studies, the overall
recurrent dislocation rate was 24% in the surgery
group and 34.6% in the conservative treatment
group. One meta-analysis found a significantly higher
rate of patellofemoral osteoarthritis in the surgery
group. There were no differences in functional
outcome scores between the conservative treatment
group and surgery group.23 Our study showed that
conservative treatment and surgical treatment were
both effective in restoring knee function at 1-year
follow-up. Nonetheless there was a trend towards
a lower rate of redislocation in the MPFL repair
surgery group, although it did not reach statistical
significance. This suggests that operative treatment
may be more beneficial for this group of patients.
In the current study, for first-time dislocators
with delayed presentation of more than 3 weeks,
conservative treatment was advised. This was
because a certain degree of healing of the torn MPFL
in the elongated position with a variable amount of
scar tissue in the gap was anticipated if the patient
presented subacutely. As the operative protocol of
direct repair of MPFL was adopted in this study, the
presence of partial healing in an elongated position
affects the decision of correct tension in the MPFL
during direct repair. As a result, a conservative
approach was adopted to minimise the possibility of
overtensioning (which might lead to medial patellofemoral
joint pain) or undertensioning (which might
lead to recurrent instability).
For recurrent patellar dislocators, studies have
shown a redislocation rate of up to 50%.1 Therefore,
it has been widely agreed that recurrent dislocation
is a strong indication for surgical treatment.24
Reconstruction of MPFL, tibial tubercle osteotomy,
and trochleoplasty have all been well-described
surgical procedures for management of recurrent
patellar dislocators. Reconstruction of MPFL alone
is indicated in the presence of a physiological
TT-TG distance (<20 mm) and no significant
trochlear dysplasia.25 Patients with increased
TT-TG distance of >15 to 20 mm have been shown
to have patellar instability.26 Thus, tibial tubercle
osteotomy procedures, aiming to shift the tibial
tubercle medially to correct the TT-TG distance
to within physiological limits of around 9 to 15 mm,
with or without concomitant MPFL reconstruction
have been advocated for these patients.25 The
cut-off point of 20 mm above which tibial tubercle
osteotomy is indicated has been well accepted by
most orthopaedic surgeons.26 27 28 29 30 One study has shown that 18% of recurrent patellar dislocators
had TT-TG distances of >20 mm.31 For patients
with significant trochlear dysplasia, trochleoplasty
procedures have been advocated.25 There have
been no prospective randomised controlled trials
to date comparing conservative treatment and the
various surgical treatment modalities for recurrent
patellar dislocators. Short-term results of these
various surgical procedures have been satisfactory,
however. Our study demonstrated similar results
to the current literature, showing a clear advantage
in terms of knee function, return to activity, and
apprehension in the MPFL reconstruction surgery
group compared with the conservative treatment
group.
There are several limitations of this study.
First, the sample size was small and a large number
of patients were lost to follow-up, making the study
underpowered. This was reflected by the non-significant
finding in the positive apprehension sign
before (88%) and 1 year (9%) after MPFL repair in
first-time dislocators (P=0.07, McNemar test).
Second, we did not adjust for confounding factors
for patellar dislocation, for example, patella alta,
increased Q-angle, and ligamentous laxity. Third,
one of the outcomes compared (apprehension sign)
was highly assessor-dependent. Although the method
of detecting apprehension sign was standardised and
the number of assessors was limited to two, potential
bias could still be introduced. In addition, no inter-observer
or intra-observer repeatability tests were
carried out. Fourth, the final assessment in the
current study was performed at 12-month follow-up.
This short follow-up may not allow adequate
evaluation of postoperative outcome. Readers of the
journal need to be aware of this during extrapolation
of the conclusion of the current study to their clinical
practice. Lastly, since there was only one recurrent
dislocator who underwent tibial tubercle osteotomy,
we are unable to conclude the results of this form of
treatment.
Conclusions
A management algorithm for patella dislocation
is presented. Repair of MPFL reduced the risk of
recurrent dislocation in first-time dislocators.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and
natural history of acute patellar dislocation. Am J Sports
Med 2004;32:1114-21. Crossref
2. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL.
Incidence of acute traumatic patellar dislocation among
active-duty United States military service members. Am J
Sports Med 2010;38:1997-2004. Crossref
3. Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations.
The natural history. Am J Sports Med 1986;14:117-20. Crossref
4. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE,
Mendelsohn C. Characteristics of patients with primary
acute lateral patellar dislocation and their recovery within
the first 6 months of injury. Am J Sports Med 2000;28:472-9.
5. Cofield RH, Bryan RS. Acute dislocation of the patella:
results of conservative treatment. J Trauma 1977;17:526-31. Crossref
6. Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation
of the patella. A correlative pathoanatomic study. Am J
Sports Med 1996;24:52-60. Crossref
7. Ahmad CS, Stein BE, Matuz D, Henry JH. Immediate
surgical repair of the medial patellar stabilizers for acute
patellar dislocation. A review of eight cases. Am J Sports
Med 2000;28:804-10.
8. Colvin AC, West RV. Patellar instability. J Bone Joint Surg
Am 2008;90:2751-62. Crossref
9. Irrgang JJ, Anderson AF, Boland AL, et al. Development
and validation of the international knee documentation
committee subjective knee form. Am J Sports Med
2001;29:600-13.
10. Tegner Y, Lysholm J. Rating systems in the evaluation
of knee ligament injuries. Clin Orthop Relat Res
1985;(198):43-9. Crossref
11. Stefancin JJ, Parker RD. First-time traumatic patellar
dislocation: a systematic review. Clin Orthop Relat Res
2007;455:93-101. Crossref
12. Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated
repair of the medial patellofemoral ligament in primary
dislocation of the patella: a prospective randomized study.
Arthroscopy 2008;24:881-7. Crossref
13. Bitar AC, Demange MK, D’Elia CO, Camanho GL.
Traumatic patellar dislocation: nonoperative treatment
compared with MPFL reconstruction using patellar
tendon. Am J Sports Med 2012;40:114-22. Crossref
14. Camanho GL, Viegas Ade C, Bitar AC, Demange MK,
Hernandez AJ. Conservative versus surgical treatment
for repair of the medial patellofemoral ligament in acute
dislocations of the patella. Arthroscopy 2009;25:620-5. Crossref
15. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. Operative
treatment of primary patellar dislocation does not improve
medium-term outcome: A 7-year follow-up report and
risk analysis of 127 randomized patients. Acta Orthop
2005;76:699-704. Crossref
16. Nikku R, Nietosvaara Y, Kallio PE, Aalto K, Michelsson JE.
Operative versus closed treatment of primary dislocation
of the patella. Similar 2-year results in 125 randomized
patients. Acta Orthop Scand 1997;68:419-23. Crossref
17. Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y.
Acute patellar dislocation in children and adolescents:
a randomized clinical trial. J Bone Joint Surg Am
2008;90:463-70. Crossref
18. Sillanpää PJ, Mäenpää HM, Mattila VM, Visuri T, Pihlajamäki H. Arthroscopic surgery for primary traumatic
patellar dislocation: a prospective, nonrandomized
study comparing patients treated with and without acute
arthroscopic stabilization with a median 7-year follow-up.
Am J Sports Med 2008;36:2301-9. Crossref
19. Sillanpää PJ, Mattila VM, Mäenpää H, Kiuru M, Visuri
T, Pihlajamäki H. Treatment with and without initial
stabilizing surgery for primary traumatic patellar
dislocation. A prospective randomized study. J Bone Joint
Surg Am 2009;91:263-73. Crossref
20. Petri M, Liodakis E, Hofmeister M, et al. Operative vs
conservative treatment of traumatic patellar dislocation:
results of a prospective randomized controlled clinical
trial. Arch Orthop Trauma Surg 2013;133:209-13. Crossref
21. Smith TO, Song F, Donell ST, Hing CB. Operative versus
non-operative management of patellar dislocation. A
meta-analysis. Knee Surg Sports Traumatol Arthrosc
2011;19:988-98. Crossref
22. Smith TO, Donell S, Song F, Hing CB. Surgical versus non-surgical
interventions for treating patellar dislocation.
Cochrane Database Syst Rev 2015;(2):CD008106. Crossref
23. Erickson BJ, Mascarenhas R, Sayegh ET, et al. Does
operative treatment of first-time patellar dislocations lead
to increased patellofemoral stability? A systematic review
of overlapping meta-analyses. Arthroscopy 2015;31:1207-15. Crossref
24. Koh JL, Stewart C. Patellar instability. Orthop Clin North
Am 2015;46:147-57. CrossRef
25. Petri M, Ettinger M, Stuebig T, et al. Current concepts for
patellar dislocation. Arch Trauma Res 2015;4:e29301. Crossref
26. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of
patellar instability: an anatomic radiographic study. Knee
Surg Sports Traumatol Arthrosc 1994;2:19-26. Crossref
27. Drexler M, Dwyer T, Dolkart O, et al. Tibial rotational
osteotomy and distal tuberosity transfer for patella
subluxation secondary to excessive external tibial torsion:
surgical technique and clinical outcome. Knee Surg Sports
Traumatol Arthrosc 2014;22:2682-9. Crossref
28. Paulos L, Swanson SC, Stoddard GJ, Barber-Westin S.
Surgical correction of limb malalignment for instability of
the patella: a comparison of 2 techniques. Am J Sports Med
2009;37:1288-300. Crossref
29. Pandit S, Frampton C, Stoddart J, Lynskey T. Magnetic
resonance imaging assessment of tibial tuberosity–trochlear groove distance: normal values for males and
females. Int Orthop 2011;35:1799-803. Crossref
30. Alemparte J, Ekdahl M, Burnier L, et al. Patellofemoral
evaluation with radiographs and computed tomography
scans in 60 knees of asymptomatic subjects. Arthroscopy
2007;23:170-7. Crossref
31. Köhlitz T, Scheffler S, Jung T, et al. Prevalence and
patterns of anatomical risk factors in patients after patellar
dislocation: a case control study using MRI. Eur Radiol
2013;23:1067-74. Crossref