Hong Kong Med J 2016 Jun;22(3):263–9 | Epub 6 May 2016
DOI: 10.12809/hkmj154645
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE CME
Common urological problems in children: prepuce, phimosis, and buried penis
Ivy HY Chan, FRCSEd(Paed), FHKAM (Surgery);
Kenneth KY Wong, PhD, FHKAM (Surgery)
Division of Paediatric Surgery, Department of Surgery, The University of Hong Kong, Queen Mary Hospital, Hong Kong
Corresponding author: Dr Kenneth KY Wong (kkywong@hku.hk)
Abstract
Parents often bring their children to the family
doctor because of urological problems. Many
general practitioners have received little training in
this specialty. In this review, we aimed to provide
a concise and informative review of common
urological problems in children. This review will
focus on the prepuce.
Introduction
Young boys are often brought by parents to see a
medical practitioner for ‘phimosis’, and circumcision
is one of the most commonly performed operations.
Yet this topic is often not taught routinely in medical
school. Buried penis is another less well-defined
condition. In this review article, we will describe
these conditions in a more systematic manner and
present the current available knowledge about the
conditions and management options.
Normal development of the prepuce and phimosis
Phimosis generally refers to a condition where the
prepuce cannot be withdrawn to expose the glans.
True phimosis, however, should be defined as a
pathological condition in which the prepuce is
scarred, non-retractile, and with a narrow preputial
ring. This is secondary to balanitis xerotica obliterans
(BXO). To avoid confusion of the terms, ‘physiological
phimosis’ and ‘pathological phimosis’ should be
used.
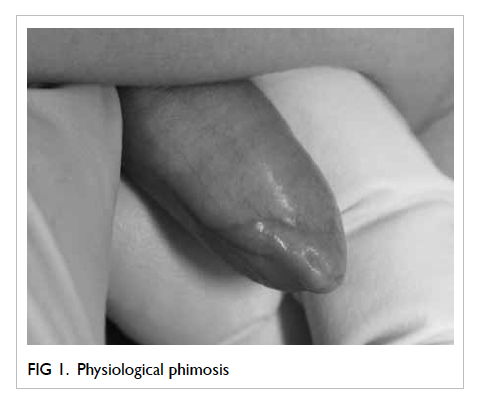
Physiological phimosis
Physiological phimosis is a natural condition in
which the prepuce cannot be retracted and there is
natural adhesion between the glans and the prepuce
(Fig 1). Almost all normal male babies are born
with a non-retractable foreskin. Indeed, Gairdner1
noticed only 4% of newborns in England and Wales
had retractable foreskin. The foreskin becomes
retractable as the child grows. The adhesion between
the prepuce and glans will also separate gradually
as a spontaneous biological process.2 3 4 By the age
of 3 years, 90% of prepuces are retractable.1 Øster2 examined preputial development in 173 Danish
boys aged 6 to 17 years annually for 7 years and
determined that the foreskin was non-retractable
in 8% of young boys but in only 1% at 17 years of
age. Similar findings were noted in Chinese boys by
Ko et al5 and Hsieh et al,6 who reported 84.1%5 and
58.1%6 of boys with a completely retractable prepuce
by the age of 13 years. Both the retractability and
the shape of the prepuce lie within a spectrum that
can sometimes be difficult to describe and there is
no agreed classification system. Different papers
have used their own classifications for the purpose
of study. One example was the study by Kayaba et
al3 in which retractability was graded according to
how much of the glans was visible after prepuce
retraction.
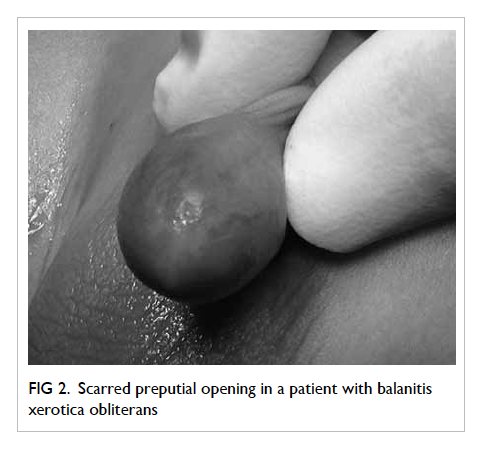
Pathological phimosis/balanitis xerotica obliterans
Balanitis xerotica obliterans is a chronic and
progressive inflammatory condition that affects the
prepuce, glans, and sometimes the urethra (Fig 2).
It was first described in 1928 by Stühmer.7 There
are three components of this condition: ‘balanitis’,
meaning chronic inflammation of the glans penis;
‘xerotica’, an abnormally dry appearance of the lesion;
and ‘obliterans’, for the association of occasional
endarteritis.
The aetiology and the true incidence is
unknown. An incidence of 0.6% has been reported
for boys affected by their 15th birthday.8 It is
suspected clinically when there is a ring of hardened
tissue with a whitish colour at the tip of the foreskin.
There are also other clinical features such as white
patches over the glans, perimeatal sclerotic changes,
or meatal stenosis. It can cause urethral stricture and
retention of urine.
Medical students are not taught about
the condition and it is generally not diagnosed at the
primary care level. Gargollo et al9 reviewed 41
patients with the pathologically confirmed diagnosis
of BXO at their centre and confirmed that no patient
had the diagnosis at referral. Pathology of the
excised prepuce showed lymphocytic infiltration in
the ripper dermis, hyalinosis and homogenisation
of collagen, basal cell vacuolation, atrophy of the
stratum malpighii, and hyperkeratosis.
Potential clinical problems
Parents often seek medical advice about their son’s
‘foreskin problems’. Pain, redness, itchiness, long
prepuce, ballooning during urination, difficulty in
retracting the prepuce, and penis being too short
are the common complaints. Before answering all
the questions, we should be able to differentiate the
normal and abnormal.
Pain, pruritus, smegma
Most parents may think that the presence of pain or
pruritus indicates infection of the prepuce, and yet
poor prepuce hygiene is a more common problem.
Smegma is another common complaint from
parents, usually described as a ‘mass’, or ‘white pearl’.
Smegma can be identified by gently retracting the
prepuce (Fig 3). It is harmless and is a combination
of secretions and desquamated skin.
Difficulty in retracting the prepuce and long prepuce
Difficulty in retracting the prepuce and long prepuce
is a feature of physiological phimosis. This is normal
in most boys and requires no attention apart from
daily routine prepuce hygiene. The role of the
physician is to differentiate normal and abnormal
prepuce, then guide proper management.
Ballooning
Ballooning is a feature of a tight prepuce. Because
of the tight preputial opening, there is dilatation of
the preputial sac during voiding. This causes a lot
of parental anxiety about possible urinary outflow
obstruction. Babu et al10 performed uroflow studies
in boys with and without ballooning of the foreskin
and determined that there was significant difference.
Balanoposthitis
This refers to inflammation of the glans (balanitis)
and the foreskin (posthitis) [Fig 4]. Patients present
with a swollen prepuce with or without discharge
from the preputial opening. It is a relatively
common condition, with a reported incidence of
6% in uncircumcised boys.11 In the absence of fever,
underlying urinary tract infection (UTI) is unlikely.
Simple bathing and rinsing with normal saline or
chlorhexidine gluconate solution after urination is
sufficient treatment for afebrile patients. Topical
antibiotic cream is commonly prescribed for local
infection. Serious conditions and presence of fever
may warrant further investigations, oral antibiotics,
or even hospital admission.
Clinical management of phimosis
Prepuce hygiene and retraction
After diagnosing physiological phimosis, parents
should be taught how to keep the prepuce clean.
Only a small proportion of parents know what is
required.12 Gentle daily retraction of the prepuce
and rinsing of the prepuce with warm water can
maintain good hygiene and prevent infection.
Parents should also be taught to avoid forcible
retraction of the prepuce.13 14 15 Simple stretching of
the prepuce alone has been shown to be effective
in achieving complete resolution of physiological
phimosis.16 After 3 months of prepuce stretching,
76% of patients reported resolution of phimosis.16
Topical steroids
Topical steroids have been prescribed in the
treatment of phimosis. Their anti-inflammatory,
immunosuppressive, and skin-thinning properties
are believed to be the mechanism for resolution of
phimosis.17 Their use in physiological phimosis was
first described by Kikiros et al.18 Subsequent studies
showed the response rate for resolution of phimosis
to be 68.2% to 95%.16 19 20 21 22 Moreno et al23 subsequently
performed a meta-analysis and reviewed 12
randomised controlled trials on the use of different
topical steroid formulations, and again confirmed the
significant benefit of corticosteroids in the complete
or partial clinical resolution of phimosis (risk
ratio=2.45; 95% confidence interval, 1.84-3.26).
Parents often ask about the potential
complications of topical steroid use. Golubovic et al24
and Pileggi et al25 addressed this issue by measuring
serum cortisol levels and salivary cortisol levels,
respectively. Neither could demonstrate a significant
change in cortisol level after application of topical
steroids. Topical steroid therapy is thus a safe and
effective alternative to circumcision.
Circumcision
Circumcision is a procedure in which part of the
foreskin is removed and results in a non-covered glans.
It is a procedure that has been described for many
years and is performed almost universally in Jewish
and Muslim boys. The rate of newborn circumcision
is high in the US (>50%),26 27 but routine circumcision is not a tradition in the Chinese population. Leung et
al28 showed the circumcision rate in 6- to 12-year-old
boys in Hong Kong to be 10.7%.
Benefits versus risks of circumcision
There is evidence that circumcision can reduce the
risk of UTI, penile cancer, human immunodeficiency
virus (HIV), and sexually transmitted disease (STD).
Urinary tract infection
Childhood UTI is associated with renal scarring. The
symptoms and signs of UTI are often non-specific in
young children who may present with fever alone. The
overall prevalence of UTI in children with fever (<19
years old) was reported to be 7.8% in a meta-analysis
published in 2008.29 The pooled prevalence of febrile
UTI in male infants from 0 to 24 months of age was
8.0% (confidence interval, 5.5-10.4%). Circumcised
boys had a lower risk of developing UTI—20.1% in
uncircumcised versus 2.4% in circumcised infants of
less than 3 months of age with fever.29
Another systematic review in 2005 showed
a decreased risk of UTI in circumcised boys.30 The
authors calculated the number-needed-to-treat was
111 in normal boys, but the number-needed-to-treat
for recurrent UTI and high-grade vesicoureteric
reflux was 11 and 4, respectively. It was evident that
the benefits of circumcision were higher for boys at
risk of UTI.
Sexually transmitted infection and human immunodeficiency virus
Three randomised controlled trials concluded that
adult circumcision had a protective effect against
acquisition of HIV.31 32 33 Although the full mechanism
of protection was not fully understood, it was
shown that the inner foreskin harbours epithelial
CD4+ CCR5+ cells and has features of an inflamed
epidermal barrier. These changes may support a
subclinical inflammatory state in uncircumcised
men, with availability of target cells for HIV
infection, and potentially account for the benefits of
circumcision in STD prevention.34 All the trials were
performed in Africa, with a much higher prevalence
of HIV. Education about use of condoms and safe
sex practice was relatively primitive compared with
Hong Kong. Readers should therefore interpret these
results with caution when discussing the benefits of
circumcision on HIV prevention with our patients.
A meta-analysis published in 2006 by Weiss
et al35 showed that circumcised males were at
a lower risk of syphilis, and there was a lower
association with herpes simplex virus (HSV) type 2. Other cohorts also showed similar findings,
with circumcised males having a decreased risk of
syphilis, gonorrhoea, and human papillomavirus
(HPV).36 37 38 39 On the contrary, another systematic
review by Van Howe40 showed that most STDs are
not impacted significantly by circumcision status.
They included chlamydia, gonorrhoea, HSV, and
HPV. Despite the positive findings in some studies,
it should be remembered that the use of a condom
and safe sex are the most important deterrents. The
protective effect of circumcision might give a false
sense of security and should not be advocated over
other preventive measures.
Risks and complications of circumcision
Circumcision is one of the most commonly
performed operations in the world and involves
excision of a ring of preputial tissue. In general, the
procedure may involve the use of a special device
(eg Plastibell, Gomco clamp, Mogen clamp, Shang
ring) or may apply the ‘free hand excision method’.
Depending on the method, suturing may or may not
be involved. Every procedure is associated with risks
and complications. The rate is different depending
on the operator (ritual circumciser or surgeon) and
the setting (home, clinic, or hospital).
There has been inadequate comparison of the
complication rates of ‘device method’ surgery and
the ‘free hand excision method’ so it is difficult for
the authors to recommend a single best method
for surgical circumcision. The overall complication
rate of circumcision varies from 0.5%41 to 8%.42 As the indication for circumcision in some patients is
not medical (eg religious or ritual circumcision), the
risks should be carefully explained to the patient
before the procedure.
Early complications include bleeding, wound
infection, and UTI. Bleeding is one of the most
common postoperative complications that, in
extreme cases, may lead to shock.43 Meticulous
technique during the procedure is thus important.
If bleeding is encountered postoperatively, it can
usually be controlled by local compression or
bedside plication.
In a UK study, the infection rate after
circumcision has been reported to be around
0.3%.44 It is usually minor and can be treated by
simple irrigation with antiseptic solution. Systemic
antibiotics are rarely needed. A systematic review of
the prevalence and complications of circumcision
was performed in eastern and southern Africa.45
The infection rate was very high and two thirds of
patients presented with systemic infection requiring
antibiotics. The authors believe the quality of local
wound care is very important in minimising the
infection rate. Urinary retention is uncommon after
circumcision but can occur in up to 3.6% of cases.
It is likely to be pain-related or due to improper
placement of a circumcision device, eg Plastibell.46
Wound dehiscence may occur and can be
managed with wound care and dressing. Very rarely,
excessive prepuce loss as a result of excessive skin
excision may be seen. This potentially disastrous
complication has been reported to be treated with a
full-thickness skin graft.47
Late complications are not uncommon,
reported by one study to be present in 4.7% of
newborn circumcisions.48 Redundant residual skin
and recurrent penile adhesion are the two most
common late complications that may necessitate
revision circumcision. Meatal stenosis is another
late but uncommon complication after circumcision
and requires surgery. The cause is not known but it
is more common in patients with BXO.49 50
There are some other less-common but severe
complications, including urethrocutaneous fistula,
glans amputation, and iatrogenic buried penis.51 52 These have long-term physiological and psychological
consequences for both the patient and family.
Surgical technique and the surgeon’s awareness
of limitations of each method of circumcision is
important. Parents should be fully informed before
they make a decision about circumcision, especially
where the patient is physically weak or where there
is no medical indication for the procedure.
Current guidelines on circumcision
Various international colleges have produced
guidelines on circumcision. These include the
British Association of Paediatric Surgeons,53 the
Royal Australasian College of Physicians,54 and the
American Academy of Pediatrics.55 56
Having taken all these into account, the overall
view of our unit is as follows:
(1) Although there is some scientific evidence for the benefits of circumcision, the routine use on all males is not justified. Parents should be fully informed of all the potential benefits and risks of the procedure.
(2) Our current medical indications for circumcision are:
(a) penile malignancy (though this is extremely rare in children) or traumatic foreskin injury where it cannot be salvaged; and
(b) BXO, severe recurrent attacks of balanoposthitis, and/or recurrent febrile UTIs.
(3) Non-therapeutic ‘ritual’ circumcision may be offered.
(1) Although there is some scientific evidence for the benefits of circumcision, the routine use on all males is not justified. Parents should be fully informed of all the potential benefits and risks of the procedure.
(2) Our current medical indications for circumcision are:
(a) penile malignancy (though this is extremely rare in children) or traumatic foreskin injury where it cannot be salvaged; and
(b) BXO, severe recurrent attacks of balanoposthitis, and/or recurrent febrile UTIs.
(3) Non-therapeutic ‘ritual’ circumcision may be offered.
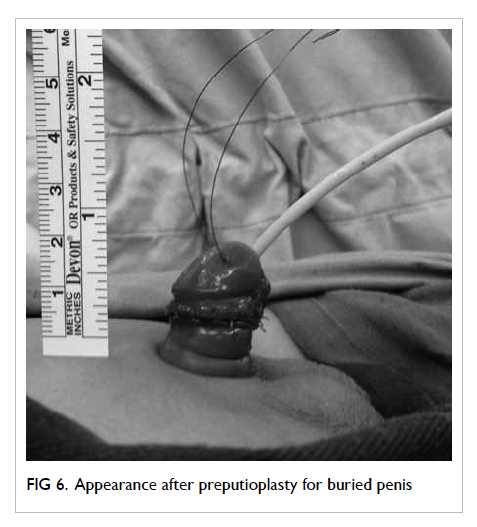
Buried penis
Buried penis is a condition where the penis is
‘trapped’ or ‘concealed’ under the suprapubic area.
There is an apparent absence or partial absence of
the penis. Figure 5 shows partial buried penis in
an 8-year-old boy. The condition was described as
‘complete’ or ‘partial’ by Crawford57 in 1977. In the
partial type, the proximal half of the penile shaft is
buried in the subcutaneous tissue. For the complete
type, the phallus is completely invisible and the glans
is covered only by prepuce. Maizels et al58 further
elaborated in 1986, offering new classifications as
‘buried penis’ (patients with redundant suprapubic
fat and/or lack of penile skin anchoring to deep fascia),
‘webbed penis’ (scrotal skin webs the penoscrotal
angle to obscure the penis), ‘trapped penis’ (the shaft
of the penis is entrapped in the scarred, prepubic
skin following trauma/overzealous circumcision),
‘micro-penis’ (a normally formed penis that is less
than two standard deviations below the mean size in
the stretched length), and ‘diminutive penis’ (a penis
that is small and/or malformed as a consequence of
epispadias/exstrophy, severe hypospadias, disorder of
sexual differentiation, or chromosomal anomalies).
O’Brien et al59 described another condition called
‘congenital megaprepuce’ in 1994 that includes
a phimotic ring and large preputial sac. Despite
these studies, buried penis is still not a well-defined
or well-classified entity. It can be congenital or
iatrogenic after overzealous circumcision. Clinicians
are reminded to examine the penis carefully and the
exact penile length should be a properly performed
‘stretched penile length’. When there is uncertainty
about the exact diagnosis, early specialist advice is
advocated.
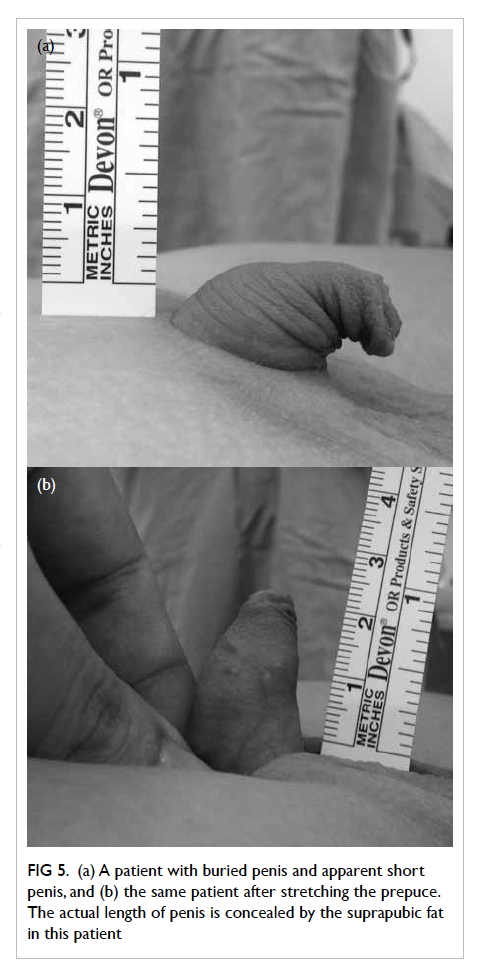
Figure 5. (a) A patient with buried penis and apparent short penis, and (b) the same patient after stretching the prepuce. The actual length of penis is concealed by the suprapubic fat in this patient
Clinical problems
For congenital problems, anxious parents usually
seek medical advice because they feel that their
child’s penis is too short. Other problems include
local infection, urinary retention, inability to void
standing, chronic urinary dripping, and undirected
voiding. For older children, there may be pain during
erection or disturbed vaginal penetration.60 61 62
Management
Anatomically, buried penis is usually due to
insufficient outer prepuce and lack of attachment
between the penile Buck’s fascia and the pubis.63
Numerous corrective surgical techniques have been
described. The underlying principle is the degloving
of the penis, anchoring of Buck’s fascia to the pubis,
and preputioplasty (pedicled preputial flap, Z-plasty
of the prepuce, lipectomy, and skin graft) [Fig 6].64 65
A study on the comparison of quality of
life before and after surgery showed significant
improvement in sexual pleasure, urination
difficulties, and genital hygiene.66 King et al61 also reported that all patients were happy with the
aesthetic results.
Conclusions
It is essential to recognise the features of physiological
versus pathological phimosis. Physiological phimosis
(tightness of prepuce), preputial adhesion, and
smegma are common and normal in young boys,
and do not require surgical intervention. There are
potential benefits and complications of circumcision
that should be thoroughly appreciated by physicians
before discussion with parents or patient. Medical
indications for circumcision include penile
malignancy, traumatic foreskin injury, recurrent
attacks of severe balanoposthitis, and recurrent
febrile UTIs with abnormal urinary tract. Very few
international societies support routine circumcision
despite the potential medical benefits incurred.
Buried penis is a condition that may warrant surgery.
References
1. Gairdner D. The fate of the foreskin, a study of circumcision.
Br Med J 1949;2:1433-7. Crossref
2. Øster J. Further fate of the foreskin. Incidence of preputial
adhesions, phimosis, and smegma among Danish
schoolboys. Arch Dis Child 1968;43:200-3. Crossref
3. Kayaba H, Tamura H, Kitajima S, Fujiwara Y, Kato T, Kato
T. Analysis of shape and retractability of the prepuce in 603
Japanese boys. J Urol 1996;156:1813-5. Crossref
4. Rickwood AM. Medical indications for circumcision. BJU
Int 1999;83 Suppl 1:45-51. Crossref
5. Ko MC, Liu CK, Lee WK, Jeng HS, Chiang HS, Li CY. Age-specific
prevalence rates of phimosis and circumcision in
Taiwanese boys. J Formos Med Assoc 2007;106:302-7. Crossref
6. Hsieh TF, Chang CH, Chang SS. Foreskin development
before adolescence in 2149 schoolboys. Int J Urol
2006;13:968-70. Crossref
7. Stühmer A. Balanitis xerotica obliterans (post operationem)
und ihre Beziehungenzur ‘Kraurosis glandi et praeputii
penis’ [in German]. Arch Dermatol Syph (Berlin) 1928;156:613. Crossref
8. Shankar KR, Rickwood AM. The incidence of phimosis in
boys. BJU Int 1999;84:101-2. Crossref
9. Gargollo PC, Kozakewich HP, Bauer SB, et al. Balanitis
xerotica obliterans in boys. J Urol 2005;174:1409-12. Crossref
10. Babu R, Harrison SK, Hutton KA. Ballooning of the
foreskin and physiological phimosis: is there any objective
evidence of obstructed voiding? BJU Int 2004;94:384-7. Crossref
11. Herzog LW, Alvarez SR. The frequency of foreskin problems
in uncircumcised children. Am J Dis Child 1986;140:254-6. Crossref
12. Osborn LM, Metcalf TJ, Mariani EM. Hygienic care in
uncircumcised infants. Pediatrics 1981;67:365-7.
13. Camille CJ, Kuo RL, Wiener JS. Caring for the
uncircumcised penis: what parents (and you) need to
know. Contemp Pediatr 2002;11:61.
14. Simpson ET, Barraclough P. The management of the
paediatric foreskin. Aust Fam Physician 1998;27:381-3.
15. Rickwood AM, Hemalatha V, Batcup G, Spitz L. Phimosis
in boys. Br J Urol 1980;52:147-50. Crossref
16. Zampieri N, Corroppolo M, Camoglio FS, Giacomello
L, Ottolenghi A. Phimosis: stretching methods with
or without application of topical steroids? J Pediatr
2005;147:705-6. Crossref
17. Kragballe K. Topical corticosteroids: mechanisms of
action. Acta Derm Venereol Suppl (Stockh) 1989;151:7-10;
discussion 47-52.
18. Kikiros CS, Beasley SW, Woodward AA. The response
of phimosis to local steroid application. Pediatr Surg Int
1993;8:329-32. Crossref
19. Lee CH, Lee SD. Effect of topical steroid (0.05% clobetasol
propionate) treatment in children with severe phimosis.
Korean J Urol 2013;54:624-30. Crossref
20. Chu CC, Chen KC, Diau GY. Topical steroid treatment of
phimosis in boys. J Urol 1999;162:861-3. Crossref
21. Orsola A, Caffaratti J, Garat JM. Conservative treatment
of phimosis in children using a topical steroid. Urology
2000;56:307-10. Crossref
22. Ghysel C, Vander Eeckt K, Bogaert GA. Long-term
efficiency of skin stretching and a topical corticoid cream
application for unretractable foreskin and phimosis in
prepubertal boys. Urol Int 2009;82:81-8. Crossref
23. Moreno G, Corbalán J, Peñaloza B, Pantoja T. Topical
corticosteroids for treating phimosis in boys. Cochrane
Database Syst Rev 2014;(9):CD008973. Crossref
24. Golubovic Z, Milanovic D, Vukadinovic V, Rakic I, Perovic
S. The conservative treatment of phimosis in boys. Br J
Urol 1996;78:786-8. Crossref
25. Pileggi FO, Martinelli CE Jr, Tazima MF, Daneluzzi JC,
Vicente YA. Is suppression of hypothalamic-pituitary-adrenal
axis significant during clinical treatment of
phimosis? J Urol 2010;183:2327-31. Crossref
26. Centers for Disease Control and Prevention (CDC). Trends
in in-hospital newborn male circumcision—United States,
1999-2010. MMWR Morb Mortal Wkly Rep 2011;60:1167-8.
27. Warner L, Cox S, Kuklina E, et al. Updated trends in
the incidence of circumcision among male newborn
delivery hospitalizations in the United States, 2000-2008.
Proceedings of the National HIV Prevention Conference;
2011 Aug 26; Atlanta, Georgia, US.
28. Leung MW, Tang PM, Chao NS, Liu KK. Hong Kong
Chinese parents’ attitudes towards circumcision. Hong
Kong Med J 2012;18:496-501.
29. Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence
of urinary tract infection in childhood: a meta-analysis.
Pediatr Infect Dis J 2008;27:302-8. Crossref
30. Singh-Grewal D, Macdessi J, Craig J. Circumcision for the
prevention of urinary tract infection in boys: a systematic
review of randomised trials and observational studies.
Arch Dis Child 2005;90:853-8. Crossref
31. Gray RH, Kigozi G, Serwadda D, et al. Male circumcision
for HIV prevention in men in Rakai, Uganda: a randomised
trial. Lancet 2007;369:657-66. Crossref
32. Bailey RC, Moses S, Parker CB, et al. Male circumcision
for HIV prevention in young men in Kisumu, Kenya: a
randomised controlled trial. Lancet 2007;369:643-56. Crossref
33. Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J,
Sitta R, Puren A. Randomized, controlled intervention trial
of male circumcision for reduction of HIV infection risk:
the ANRS 1265 Trial. PLoS Med 2005;2:e298. Crossref
34. Lemos MP, Lama JR, Karuna ST, et al. The inner foreskin
of healthy males at risk of HIV infection harbors epithelial
CD4+ CCR5+ cells and has features of an inflamed
epidermal barrier. PLoS One 2014;9:e108954. Crossref
35. Weiss HA, Thomas SL, Munabi SK, Hayes RJ. Male
circumcision and risk of syphilis, chancroid, and genital
herpes: a systematic review and meta-analysis. Sex Transm
Infect 2006;82:101-9; discussion 110. Crossref
36. Diseker RA 3rd, Peterman TA, Kamb ML, et al.
Circumcision and STD in the United States: cross sectional
and cohort analyses. Sex Transm Infect 2000;76:474-9. Crossref
37. Albero G, Castellsagué X, Giuliano AR, Bosch FX. Male
circumcision and genital human papillomavirus: a
systematic review and meta-analysis. Sex Transm Dis
2012;39:104-13. Crossref
38. Tobian AA, Serwadda D, Quinn TC, et al. Male
circumcision for the prevention of HSV-2 and HPV
infections and syphilis. N Engl J Med 2009;360:1298-309. Crossref
39. Turner AN, Morrison CS, Padian NS, et al. Male
circumcision and women’s risk of incident chlamydial,
gonococcal, and trichomonal infections. Sex Transm Dis
2008;35:689-95. Crossref
40. Van Howe RS. Sexually transmitted infections and male
circumcision: a systematic review and meta-analysis. ISRN
Urol 2013;2013:109846. Crossref
41. El Bcheraoui C, Zhang X, Cooper CS, Rose CE, Kilmarx
PH, Chen RT. Rates of adverse events associated with male
circumcision in U.S. medical settings, 2001 to 2010. JAMA
Pediatr 2014;168:625-34. Crossref
42. Weiss HA, Larke N, Halperin D, Schenker I. Complications
of circumcision in male neonates, infants and children: a
systematic review. BMC Urol 2010;10:2. Crossref
43. Bocquet N, Chappuy H, Lortat-Jacob S, Chéron G. Bleeding
complications after ritual circumcision: about six children.
Eur J Pediatr 2010;169:359-62. Crossref
44. Cathcart P, Nuttall M, van der Meulen J, Emberton M,
Kenny SE. Trends in paediatric circumcision and its
complications in England between 1997 and 2003. Br J
Surg 2006;93:885-90. Crossref
45. Wilcken A, Keil T, Dick B. Traditional male circumcision
in eastern and southern Africa: a systematic review of
prevalence and complications. Bull World Health Organ
2010;88:907-14. Crossref
46. Mihssin N, Moorthy K, Houghton PW. Retention of urine:
an unusual complication of the Plastibell device. BJU Int
1999;84:745. Crossref
47. Özdemir E. Significantly increased complication risks with
mass circumcisions. Br J Urol 1997;80:136-9. Crossref
48. Patel HI, Moriarty KP, Brisson PA, Feins NR. Genitourinary
injuries in the newborn. J Pediatr Surg 2001;36:235-9. Crossref
49. Pieretti RV, Goldenstein AM, Pieretti-Vanmarcke R. Late
complications of newborn circumcision: a common and
avoidable problem. Pediatr Surg Int 2010;26:515-8. Crossref
50. Homer L, Buchanan KJ, Nasr B, Losty PD, Corbett
HJ. Meatal stenosis in boys following circumcision for
lichen sclerosus (balanitis xerotica obliterans). J Urol
2014;192:1784-8. Crossref
51. Ceylan K, Burhan K, Yilmaz Y, Can S, Kuş A, Mustafa G.
Severe complications of circumcision: an analysis of 48
cases. J Pediatr Urol 2007;3:32-5. Crossref
52. Ince B, Gundeslioglu AO. A salvage operation for total
penis amputation due to circumcision. Arch Plast Surg
2013;40:247-50. Crossref
53. Management of foreskin conditions. British Association
of Paediatric Surgeons. Available from: http://www.baps.org.uk/resources/documents/management-foreskin-conditions/.
Accessed Jun 2015.
54. The Royal Australasian College of Physicians. Circumcision
of infant males. 2010. Available from: https://www.racp.edu.au/docs/default-source/advocacy-library/circumcision-of-infant-males.pdf. Accessed Jun 2015.
55. American Academy of Pediatrics Task Force on
Circumcision. Circumcision policy statement. Pediatrics
2012;130:585-6. Crossref
56. American Academy of Pediatrics Task Force on
Circumcision. Male circumcision. Pediatrics
2012;130:e756-85. Crossref
57. Crawford BS. Buried penis. Br J Plast Surg 1977;30:96-9. Crossref
58. Maizels M, Zaontz M, Donovan J, Bushnick PN, Firlit
CF. Surgical correction of the buried penis: description
of a classification system and a technique to correct the
disorder. J Urol 1986;136:268-71.
59. O’Brien A, Shapiro AM, Frank JD. Phimosis or congenital
megaprepuce? Br J Urol 1994;73:719-20. Crossref
60. Mattsson B, Vollmer C, Schwab C, et al. Complications of
a buried penis in an extremely obese patient. Andrologia
2012;44 Suppl 1:826-8. Crossref
61. King IC, Tahir A, Ramanathan C, Siddiqui H. Buried
penis: evaluation of outcomes in children and adults,
modification of a unified treatment algorithm, and review
of the literature. ISRN Urol 2013;2013:109349. Crossref
62. Donatucci CF, Ritter EF. Management of the buried penis
in adults. J Urol 1998;159:420-4. Crossref
63. Chin TW, Tsai HL, Liu CS. Modified prepuce unfurling for
buried penis: a report of 12 years of experience. Asian J
Surg 2015;38:74-8. Crossref
64. Liu X, He DW, Hua Y, Zhang DY, Wei GH. Congenital
completely buried penis in boys: anatomical basis and
surgical technique. BJU Int 2013;112:271-5. Crossref
65. Chu CC, Chen YH, Diau GY, Loh IW, Chen KC. Preputial
flaps to correct buried penis. Pediatr Surg Int 2007;23:1119-21. Crossref
66. Hughes DB, Perez E, Garcia RM, Aragón OR, Erdmann
D. Sexual and overall quality of life improvements after
surgical correction of “buried penis”. Ann Plast Surg
2016;76:532-5. Crossref