Hong Kong Med J 2015 Dec;21(6):518–23 | Epub 11 Sep 2015
DOI: 10.12809/hkmj144456
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Childhood intussusception: 17-year experience at a tertiary referral centre in Hong Kong
Carol WY Wong, MB, BS, MRCSEd1;
Ivy HY Chan, MB, BS, FHKAM (Surgery)1;
Patrick HY Chung, MB, BS, FHKAM (Surgery)1;
Lawrence CL Lan, MB, BS, FHKAM (Surgery)1;
Wendy WM Lam, MB, BS, FHKAM (Radiology)2;
Kenneth KY Wong, PhD, FHKAM (Surgery)1;
Paul KH Tam, ChM, FHKAM (Surgery)1
1 Department of Surgery, The University of Hong Kong, Queen Mary Hospital, Pokfulam, Hong Kong
2 Department of Radiology, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Prof Kenneth KY Wong (kkywong@hku.hk)
Abstract
Objectives: To review all paediatric patients with
intussusception over the last 17 years.
Design: Retrospective case series.
Setting: A tertiary centre in Hong Kong.
Patients: Children who presented with
intussusception from January 1997 to December
2014 were reviewed.
Main outcome measures: The duration of
symptoms, successful treatment modalities,
complication rate, and length of hospital stay were
studied.
Results: A total of 173 children (108 male, 65 female)
presented to our hospital with intussusception
during the study period. Their median age at
presentation was 12.5 months (range, 2 months to
16 years) and the mean duration of symptoms was
2.3 (standard deviation, 1.8) days. Vomiting was
the most common symptom (76.3%) followed by
abdominal pain (46.2%), per rectal bleeding or red
currant jelly stool (40.5%), and a palpable abdominal
mass (39.3%). Overall, 160 patients proceeded to
pneumatic or hydrostatic reduction, among whom
127 (79.4%) were successful. Three (1.9%) patients
had bowel perforation during the procedure. Early
recurrence of intussusception occurred in four
(3.1%) patients with non-operative reduction. No
recurrence was reported in the operative group. The
presence of a palpable abdominal mass was a risk
factor for operative treatment (relative risk=2.0; 95%
confidence interval, 1.8-2.2). Analysis of our results
suggested that duration of symptoms did not affect
the success rate of non-operative reduction.
Conclusions: Non-operative reduction has a high
success rate and low complication rate, but the
presence of a palpable abdominal mass is a risk
factor for failure. Operative intervention should not
be delayed in those patients who encounter difficult
or doubtful non-operative reduction.
New knowledge added by this
study
- Non-operative reduction of intussusception has a high success rate and low complication rate, even in delayed presentation of over 72 hours.
- The presence of a palpable abdominal mass is a risk factor for failure of non-operative reduction.
- Non-operative reduction is recommended as the first-line treatment for children with intussusception.
- Operative intervention should not be delayed in those patients who encounter difficult or doubtful non-operative reduction.
Introduction
Intussusception is the most common cause of
intestinal obstruction in infants and young children
between the age of 3 months and 3 years, and the
peak age of presentation is 4 to 8 months.1 The
invagination of proximal bowel into more distal
bowel results in venous congestion and bowel wall
oedema. If this condition is not promptly diagnosed
and treated, arterial obstruction and bowel necrosis
and perforation may occur.2 Approximately 90% of
intussusceptions in the paediatric age-group are
ileocolic and idiopathic,3 presumably caused by
lymphoid hyperplasia that has been suggested as the
‘lead point’ in its pathogenesis.4 Viral infection may
also play a role.5 6 7 8
The reported incidence of a pathological
lead point in paediatric intussusception is
approximately 6%,9 the most common of which
is Meckel’s diverticulum.10 Systemic conditions
such as Henoch-Schönlein purpura, Peutz-Jeghers
syndrome, and familial polyposis can also increase
the risk of intussusception. Abdominal trauma and
postoperative abdomen have also been reported to
pose a higher risk for intussusception.11 12 13 14
The presenting symptoms of intussusception
are often non-specific and may mimic viral gastro-enteritis,
presenting as vomiting and diarrhoea. The
classic triad of red currant jelly stool, abdominal
pain, and abdominal mass is not often encountered,
and the diagnosis may easily be delayed or missed.15
Plain abdominal films are neither sensitive nor
specific for intussusception and may be completely
normal.16 The most consistent finding is a paucity of
gas in the right iliac fossa. Other possible features
include soft tissue mass, target sign, or meniscus
sign.17 The first-line investigation for diagnosis of
intussusception in children is abdominal ultrasound,
given its high sensitivity (98%-100%) and specificity
(88%-100%).18
Non-operative reduction methods for
intussusception include barium enema, and
hydrostatic or pneumatic reduction.19 Pneumatic
reduction is currently the preferred standard
treatment, given the greater ease of performing
the examination, the lesser morbidity with
complications, and the slightly higher success rate of
84% to 100%.20 21 22
Operative reduction is required when non-operative
reduction is either contra-indicated
(eg peritonitis, perforation, profound shock) or
unsuccessful. Open surgery has been the conventional
approach although laparoscopic reduction is also
feasible and successful in uncomplicated cases.23 24
In this study, we aimed to review our hospital’s
experience in the management of paediatric
intussusception over the last 17 years, with a focus
on assessing the efficacy of non-operative reduction
and identifying the risk factors that may lower its
success rate.
Methods
We conducted a retrospective study of children who
presented with intussusception from January 1997 to
December 2014 in our hospital. We started with the
year 1997 as some of earlier records were incomplete.
Patient demographics, clinical presentation,
duration of symptoms, treatment modalities,
complication rate, and length of hospital stay were
studied. The method of non-operative reduction in
our institution was ultrasound-guided hydrostatic
reduction before 2005 and pneumatic reduction
with fluoroscopy after 2005, as the latter was easier
and faster to perform. The procedure was performed
by paediatric radiologists, with a paediatric surgeon
available if necessary. In pneumatic reduction, air
is insufflated via a Foley catheter (with size of 18-Fr
to 22-Fr, depending on patient’s size, with balloon
inflated with 10 mL water) placed inside the patient’s
rectum under pressure monitoring at 120 mm Hg.
Our radiologists would perform a maximum of three
attempts. The patient might be given intravenous
midazolam at a dose of 0.1 to 0.2 mg/kg if necessary.
Successful reduction was demonstrated by free flow of
air into the terminal ileum and disappearance of the
caecal soft tissue mass.
For laparoscopic reduction, a 5-mm subumbilical
port was used for camera access. Another
two working ports (one in the upper and one in
the lower abdomen) were inserted. Reduction of
intussusception was performed with laparoscopic
graspers. In open reduction, manual reduction was
achieved by milking the intussusceptum out of the
intussuscipient. Bowel resection was performed
when bowel necrosis was found intra-operatively.
Data analysis was carried out using the
Statistical Package for the Social Sciences (Windows
version 21.0; SPSS Inc, Chicago [IL], US). Mean values
were expressed with standard deviation. Continuous
variables were compared with Mann-Whitney U
test and categorical values with Chi squared test.
Results were considered statistically significant
when P≤0.05. Comparison of success, recurrence,
and complication rates between hydrostatic and
pneumatic reduction groups was performed. The
length of hospital stay was also compared.
Results
A total of 173 children (108 male, 65 female)
presented to our hospital with intussusception
during the study period. Of them, 83 (48%) were
admitted directly to our paediatric surgical ward, 50
(29%) were referred from the paediatric medical ward
in our hospital, and the remaining 40 (23%) were
referred from other public and private hospitals. The
median age at presentation was 12.5 months (range,
2 months to 16 years) and the mean (± standard
deviation) duration of presenting symptoms was 2.3
± 1.8 days. The common presenting symptoms and
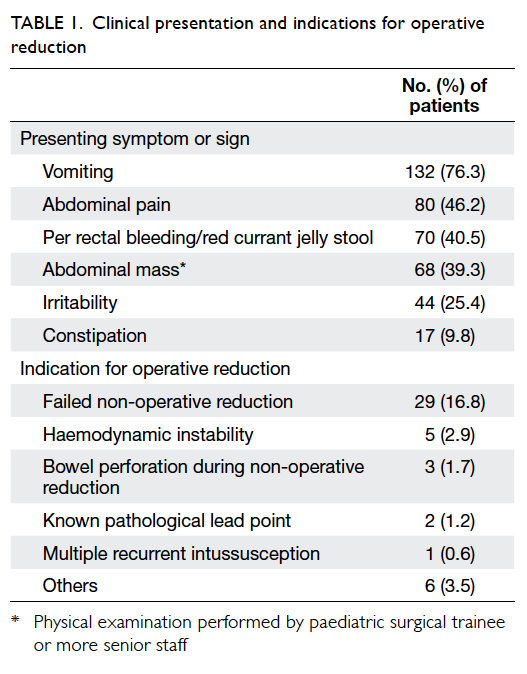
their percentage of occurrence are shown in Table 1. The most common symptom reported was vomiting
and occurred in 132 (76.3%) patients.
All patients except one were diagnosed by
ultrasonography. One patient underwent computed
tomographic scan for diagnosis due to an atypical
presentation of intussusception. All patients
underwent either non-operative or operative
treatment within 24 hours of admission. Pneumatic
or hydrostatic reduction (Fig a) was performed in 160 patients, among which 127 (79.4%) were
successful and three (1.9%) were complicated by
bowel perforation. A total of 46 patients in our
study required operative reduction, but two of the
intussusceptions were found to be reduced upon
laparotomy. These radiological misdiagnoses could
be due to mistaken identity of the oedematous
ileocaecal valve for intussusceptum. The indications
for operative treatment are summarised in Table 1. Early recurrence of intussusception (<72 hours
post-reduction) occurred in four (3.1%) of the 127
patients who had initial successful non-operative
reduction. No recurrence was reported in patients
treated surgically. Laparoscopic reduction was
attempted in 13 patients, among whom five (38.5%)
were successful. Conversion to open reduction was
required in five patients because of the need for
bowel resection and in a further three due to difficult
reduction. Among the 46 patients who required
operative reduction, 23 (50%) required bowel
resection. A pathological lead point was noted intra-operatively
in seven (15.2%) patients and four had a
perforated bowel (three of which were complications
of non-operative reduction). The remaining 12 had
non-viable gangrenous bowel that was subsequently
confirmed by histology. The operations were
complicated with one burst abdomen and one
anastomotic leak. The age distribution in our
cohort of patients and the number of patients with
pathological lead point are shown in Table 2.
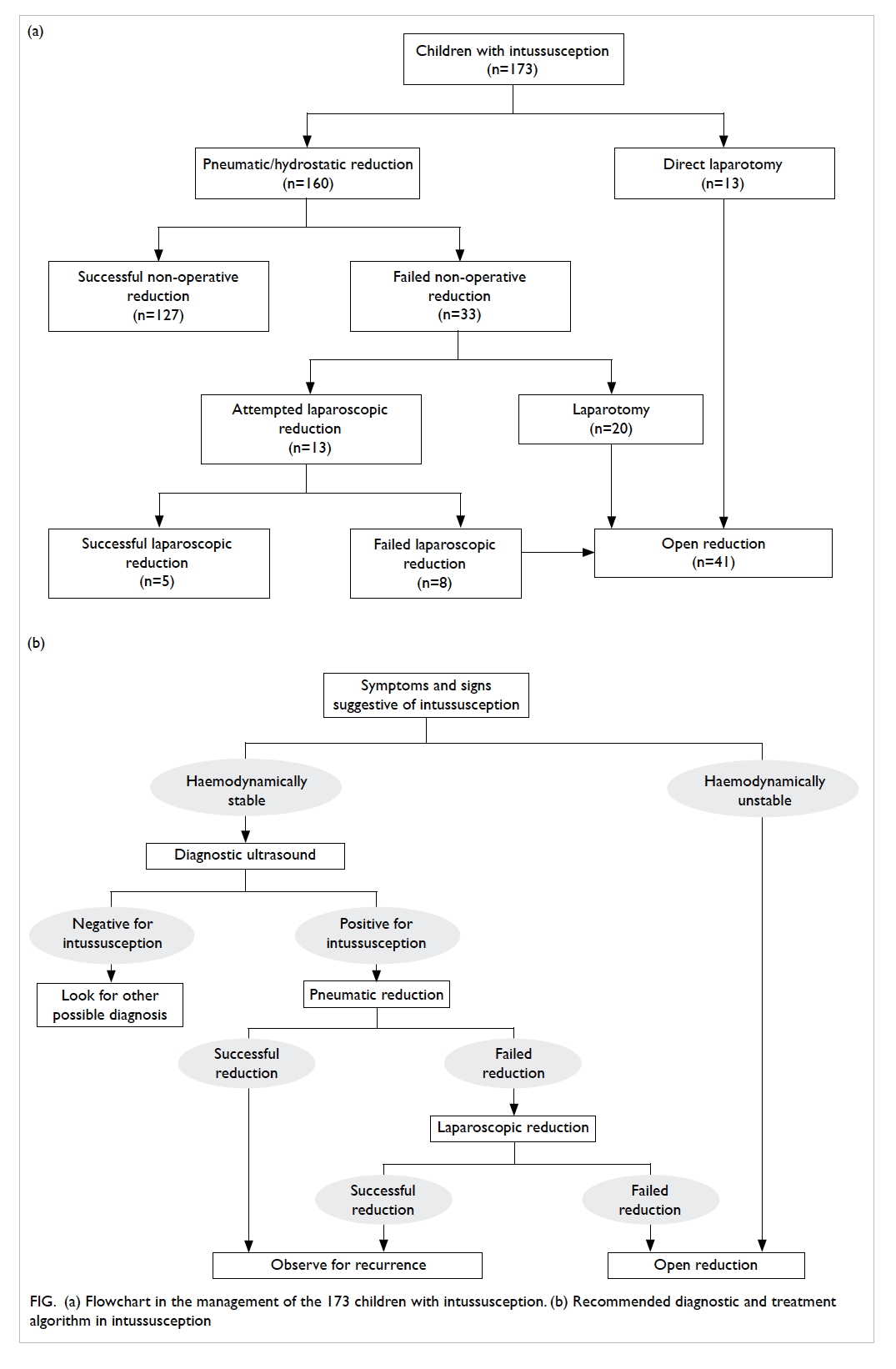
Figure. (a) Flowchart in the management of the 173 children with intussusception. (b) Recommended diagnostic and treatment algorithm in intussusception
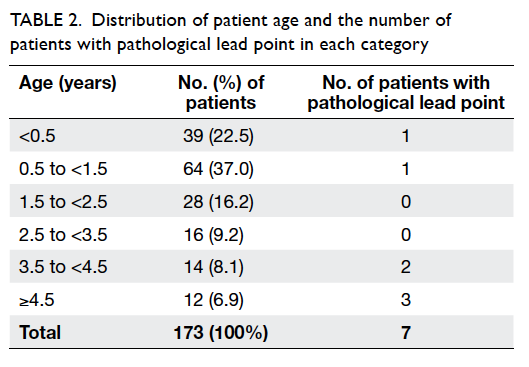
Table 2. Distribution of patient age and the number of patients with pathological lead point in each category
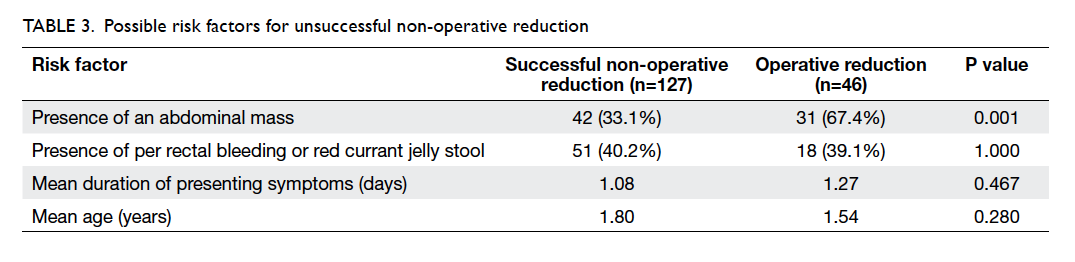
We next analysed the possible risk factors for
unsuccessful non-operative reduction in the 160
patients (Table 3). The only statistically significant
factor was the presence of an abdominal mass
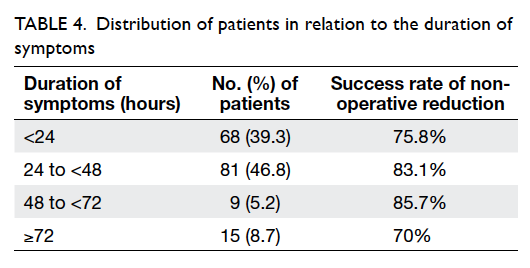
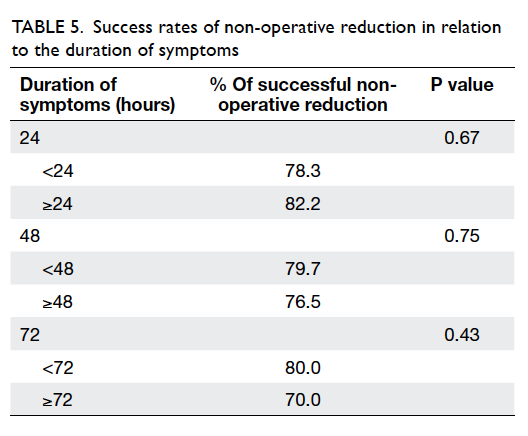
(relative risk=2.0; 95% confidence interval, 1.8-2.2). The distribution of the duration of symptoms
is presented in Table 4. Nonetheless, the duration
of symptoms and the extent of the intussusception
did not appear to affect the chance of a successful
non-operative reduction (Table 5). There were 129
patients with intussusception at the hepatic flexure
or a more proximal site, 93 (72.1%) of whom had
successful non-operative reduction; 44 presented
with intussusception at the transverse colon or a
more distal site, of whom 34 (77.3%) underwent
successful non-operative reduction. There was
no significant difference in the success rate of
non-operative reduction between the two groups
(P=0.56). Approximately 50% of patients were
admitted directly to our ward from the beginning.
There was no difference in the success rate of non-operative
reduction between this group of patients
and those who were referred from other wards or
hospitals (77.1% vs 77.3%, P=1.00).
The overall success rate of non-operative
reduction was 79.4%. We also compared the success
rate for the two non-operative treatment modalities.
There was no statistically significant difference
between the success rate of hydrostatic reduction
(81.5%) versus pneumatic reduction (77.2%) in our
study (P=0.56).
There was a statistically significant difference
in the median length of post-reduction hospital stay
for patients who were successfully treated non-operatively
(3 days; range, 1-12 days) versus operatively
(7.5 days; range, 3-73 days; P=0.01).
Discussion
Intussusception is a true paediatric surgical
emergency and is second only to appendicitis as
the most common cause of an acute abdominal
emergency in children.25 The complete classic triad of
intermittent abdominal pain, red currant jelly stool,
and a palpable abdominal mass is not a common
presentation.26 Only five (2.9%) of our patients were
documented to have all three symptoms present at
the time of hospital admission. In accordance with
previous studies, vomiting was the most common
presenting symptom.4 27 Per rectal bleeding or red
currant jelly stool signify bowel ischaemia and
mucosal sloughing but is a rather late sign and was
present in only 40.5% of our patients. Nonetheless, all
except one patient had at least one of the symptoms
of abdominal pain, abdominal mass, red currant
jelly stool, vomiting, or irritability. These symptoms
should be actively sought in any patient in whom
intussusception is suspected.
The most reliable abdominal sign, if present, is
a palpable mass in the right upper quadrant of the
abdomen. It was present in 39.3% of our patients,
and was a risk factor for the need of operative
treatment. We postulate that a palpable mass may
signify relatively longer duration of intussusception
that causes complete intestinal obstruction, thus
rendering non-operative reduction less successful as
it becomes more difficult for the reduction medium
to pass through. Many children with intussusception
present with non-specific signs and symptoms, thus
the diagnosis may easily be delayed or missed.15
Therefore, as clinicians we must maintain a high
index of suspicion in order to identify this emergency
in a timely manner. Early referral of suspected cases
to a tertiary treatment centre can significantly reduce
morbidity in the child.
With positive sonographic findings of
intussusception, an enema is reserved for therapeutic
purposes, although it may be necessary for diagnosis
when ultrasonography findings are questionable.
Computed tomography is seldom needed for
diagnosis of paediatric intussusception, except in
cases where an associated underlying pathological
lead point is suspected. Our recommended diagnostic
and treatment algorithm is summarised in Figure b. Pneumatic reduction is currently our preferred
standard treatment of intussusception, given the
greater ease of performing the examination, lesser
morbidity with complication, and the high success
rate.20 21 22 Major advantages of air enema reduction
include a relatively low radiation dose and improved
safety with constant pressure monitoring.28 29 The
perforation rate is reported to be less than 3%.30
In a randomised trial performed by Hadidi and El
Shal,22 pneumatic reduction was concluded to be
the modality with fewest complications and highest
success rate, when compared with barium enema
and hydrostatic reduction. In our study, there was
no statistically significant difference in the success
rate between hydrostatic reduction and pneumatic
reduction (81.5% vs 77.2%, P=0.56). We believe that
this is attributable to the fact that both hydrostatic
and pneumatic reductions are based on similar
principles.
Laparoscopic reduction has been demonstrated
to be feasible and successful in uncomplicated
intussusception.23 24 In our series, five (62.5%) of
the eight conversions from laparoscopic to open
reduction were due to the need for bowel resection.
Non-operative reduction has a high overall
success rate and low complication and recurrence
rates. A high success rate was observed even in the
group of patients with delayed presentation of over
72 hours. It also leads to a shorter hospital stay and
is therefore recommended as the first-line treatment
of this condition.
The presence of a palpable abdominal mass is
a risk factor for failure of non-operative reduction.
Operative intervention should not be delayed in
these patients who encounter difficult or doubtful
non-operative reduction. For patients in whom non-operative
reduction fails, laparoscopic reduction
appears to be a feasible option. From our experience,
a significant proportion of this group of patients
require bowel resection. If the viability of the bowel
is doubtful during laparoscopy, early conversion to
open surgery should be performed in order to avoid
delay in treatment.
Conclusions
Non-operative reduction has a high success rate and
low complication rate, but the presence of a palpable
abdominal mass is a risk factor for failure. Operative
intervention should not be delayed in these patients
who encounter difficult or doubtful non-operative
reduction.
References
1. Bines J, Ivanoff B. Acute intussusception in infants and
children: incidence, clinical presentation and management: a global perspective. Report 02.19. Geneva: World Health
Organization; 2002.
2. Stringer MD, Pablot SM, Brereton RJ. Paediatric
intussusception. Br J Surg 1992;79:867-76. Crossref
3. Bajaj L, Roback MG. Postreduction management of
intussusception in a children’s hospital emergency
department. Pediatrics 2003;112:1302-7. Crossref
4. DiFiore JW. Intussusception. Semin Pediatr Surg
1999;8:214-20. Crossref
5. Mayell MJ. Intussusception in infancy and childhood in
Southern Africa. A review of 223 cases. Arch Dis Child
1972;47:20-5. Crossref
6. Mangete ED, Allison AB. Intussusception in infancy
and childhood: an analysis of 69 cases. West Afr J Med
1994;13:87-90.
7. Asano Y, Yoshikawa T, Suga S, Hata T, Yamazaki T, Yazaki
T. Simultaneous occurrence of human herpesvirus 6
infection and intussusception in three infants. Pediatr
Infect Dis J 1991;10:335-7. Crossref
8. O’Ryan M, Lucero Y, Peña A, Valenzuela MT. Two year review
of intestinal intussusception in six large public hospitals of
Santiago, Chile. Pediatr Infect Dis J 2003;22:717-21. Crossref
9. Blakelock RT, Beasley SW. The clinical implications of non-idiopathic
intussusception. Pediatr Surg Int 1998;14:163-7. Crossref
10. Navarro O, Dugougeat F, Kornecki A, Shuckett B, Alton DJ,
Daneman A. The impact of imaging in the management of
intussusception owing to pathologic lead points in children.
A review of 43 cases. Pediatr Radiol 2000;30:594-603. Crossref
11. Komadina R, Smrkolj V. Intussusception after blunt
abdominal trauma. J Trauma 1998;45:615-6. Crossref
12. Stockinger ZT, McSwain N Jr. Intussusception caused by
abdominal trauma: case report and review of 91 cases
reported in the literature. J Trauma 2005;58:187-8. Crossref
13. Türkyilmaz Z, Sönmez K, Demiroğullari B, et al. Postoperative
intussusception in children. Acta Chir Belg 2005;105:187-9.
14. Emil S, Shaw X, Laberge JM. Post-operative colocolic
intussusception. Pediatr Surg Int 2003;19:220-2.
15. Reijnen JA, Festen C, Joosten HJ, van Wieringen PM.
Atypical characteristics of a group of children with
intussusception. Acta Paediatr Scand 1990;79:675-9. Crossref
16. Hernandez JA, Swischuk LE, Angel CA. Validity of plain
films in intussusception. Emerg Radiol 2004;10:323-6.
17. Ratcliffe JF, Fong S, Cheong I, O’Connell P. The plain
abdominal film in intussusception: the accuracy and incidence
of radiographic signs. Pediatr Radiol 1992;22:110-1. Crossref
18. Bhisitkul DM, Listernick R, Shkolnik A, et al. Clinical
application of ultrasonography in the diagnosis of
intussusception. J Pediatr 1992;121:182-6. Crossref
19. Peh WC, Khong PL, Lam C, et al. Reduction of
intussusception in children using sonographic guidance.
AJR Am J Roentgenol 1999;173:985-8. Crossref
20. Lui KW, Wong HF, Cheung YC, et al. Air enema for
diagnosis and reduction of intussusception in children:
clinical experience and fluoroscopy time correlation. J
Pediatr Surg 2001;36:479-81. Crossref
21. Rubí I, Vera R, Rubí SC, et al. Air reduction of
intussusception. Eur J Pediatr Surg 2002;12:387-90. Crossref
22. Hadidi AT, El Shal N. Childhood intussusception: a
comparative study of nonsurgical management. J Pediatr
Surg 1999;34:304-7. Crossref
23. Schier F. Experience with laparoscopy in the treatment of
intussusception. J Pediatr Surg 1997;32:1713-4. Crossref
24. Poddoubnyi IV, Dronov AF, Blinnikov OI, Smirnov AN,
Darenkov IA, Dedov KA. Laparoscopy in the treatment of
intussusception in children. J Pediatr Surg 1998;33:1194-7. Crossref
25. Waseem M, Rosenberg HK. Intussusception. Pediatr
Emerg Care 2008;24:793-800. Crossref
26. Bruce J, Huh YS, Cooney DR, Karp MP, Allen JE, Jewett
TC Jr. Intussusception: evolution of current management. J
Pediatr Gastroenterol Nutr 1987;6:663-74. Crossref
27. Losek JD. Intussusception: don’t miss the diagnosis! Pediatr
Emerg Care 1993;9:46-51. Crossref
28. Stringer DA, Ein SH. Pneumatic reduction: advantages,
risks and indications. Pediatr Radiol 1990;20:475-7. Crossref
29. Meyer JS, Dangman BC, Buonomo C, Berlin JA. Air and
liquid contrast agents in the management of intussusception:
a controlled, randomized trial. Radiology 1993;188:507-11. Crossref
30. Daneman A, Alton DJ, Ein S, Wesson D, Superina R,
Thorner P. Perforation during attempted intussusception
reduction in children—a comparison of perforation with
barium and air. Pediatr Radiol 1995;25:81-8. Crossref