Hong Kong Med J 2014 Aug;20(4):285–9 | Epub 14 March 2014
DOI: 10.12809/hkmj134061
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Severe acute pyelonephritis: a review of clinical outcome and risk factors for mortality
Vera Y Chung, FHKAM (Surgery), FRCS (Edin);
CK Tai, FHKAM (Surgery), FRCS (Edin);
CW Fan, FHKAM (Surgery), FRCS (Edin);
CN Tang, FHKAM (Surgery), FRCS (Edin)
Division of Urology, Department of Surgery, Pamela Youde Nethersole
Eastern Hospital, Chai Wan, Hong Kong
Corresponding author: Dr VY Chung (chungyeungvera@gmail.com)
Abstract
Objective: To review demographics of patients with acute pyelonephritis, their outcomes of severe upper urinary tract infection,
and to identify risk factors for long hospital stay and
mortality.
Design: Case series.
Setting: A regional hospital in Hong Kong.
Patients: Patients admitted between June 2007 and
June 2012 for acute pyelonephritis were identified.
Those with the most severe outcomes were analysed
of their mortality, need for care in the intensive care
unit, or necessitation of urological intervention.
Results: Overall, 68 patients fulfilled our criteria
for severe acute pyelonephritis. The female-to-male
ratio was 7:3. Their mean age was 58 years. Overall,
57% of the patients had impaired renal function
and 37% were diabetic; 47% developed shock after
admission and 56% required further intensive
care unit care; 75% of the patients demonstrated
radiological evidence of urinary tract obstruction
and required subsequent drainage procedures. Five
patients died due to severe acute pyelonephritis. The
prevalence of bacteraemia and bacteriuria was 57%
and 74%, respectively. Escherichia coli accounted
for the majority of causative organisms. Four risk
factors—bacteraemia, shock, need for
intensive care, and suppurative pyelonephritis—were associated with hospital stay of longer than 14
days. Old age (≥65 years), male sex, deranged renal
function, and presence of disseminated intravascular
coagulation were associated with mortality.
Conclusion: There was high prevalence of
bacteraemia and septic shock in patients with
severe acute pyelonephritis. The factors of old age
(≥65 years), male sex, deranged renal function, and
presence of disseminated intravascular coagulation
were associated with mortality. With the support
of intensive care, early recognition of urinary tract
obstruction and timely drainage, patients with
severe acute pyelonephritis generally carry a good
prognosis.
New knowledge added by this
study
- Contrary to the usual belief, the complexity of renal infections and septic shock were predictors for long hospital stay but not mortality.
- Escherichia coli still accounts for the majority of causative organisms in hospitalised patients with severe acute pyelonephritis.
- Early recognition of urinary tract obstruction and timely drainage are important in the treatment of severe acute pyelonephritis.
- Physicians could prevent potential mortalities by identifying those with risk factors and providing early intervention and intensive care.
Introduction
Acute pyelonephritis (AP) represents the most
severe form of urinary tract infection (UTI) and
is associated with significant morbidity and even
mortality. Approximately 250 000 cases of AP occur
each year in the US, with the incidence being higher
in women than men.1 The aetiological agent is
Escherichia coli in around 80% of the cases.2 Acute pyelonephritis has a quoted mortality of 10% to 20%.3
Several studies have identified a number of risk
factors for prediction of poor outcome, including
urinary tract abnormality, general debility, and
properties (ie virulence and resistance profile) of
microorganisms.4 5
The aim of this study was to review patient
demographics and outcomes of severe AP in a regional hospital, and to identify possible prognostic
factors for long hospital stay and fatal events.
Methods
Study design and data collection
We conducted a retrospective medical record review.
All patients admitted for AP between June 2007
and June 2012 to Pamela Youde Nethersole Eastern
Hospital, Hong Kong were identified. Only patients
with the most severe outcomes were analysed
consecutively: (1) mortality, (2) need for care in
the intensive care unit (ICU), or (3) necessitation
of urological intervention. Patients suffering from
postoperative pyelonephritis were excluded.
The following data were collected: patient
demographics, presence of urinary tract obstruction,
presence of septic shock, need for intensive care,
modalities of urological intervention, bacteriologies,
length of stay, and mortality.
Statistical analysis
Data analysis was performed by the Statistical Package
for the Social Sciences (Windows version 20; SPSS
Inc, Chicago [IL], US). A P value of less than 0.05 was
regarded as statistically significant. Chi squared test
and logistic regression analysis were performed. The
independent variables were patients’ demographic
and clinical data; the dependent variables were
mortality and long hospital stay (>14 days).
Results
Patient characteristics
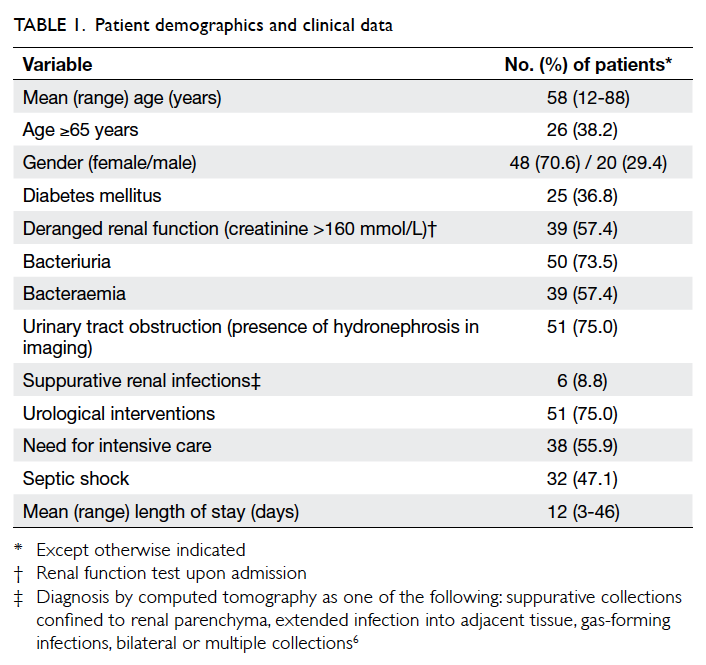
A total of 432 patients were admitted for AP from
June 2007 to June 2012. Of these, 68 patients fulfilled
our inclusion criteria for severe AP. Baseline patient
demographics, clinical characteristics, and imaging
findings are illustrated in Table 1.6 Overall, 75.0%
of the patients (n=51) demonstrated radiological
evidence of urinary tract obstruction, secondary to
stone (51.0%), ureteral stricture (5.8%), or extrinsic
compression (7.2%). Six patients had suppurative
renal infections, namely, renal abscess and
emphysematous pyelonephritis.
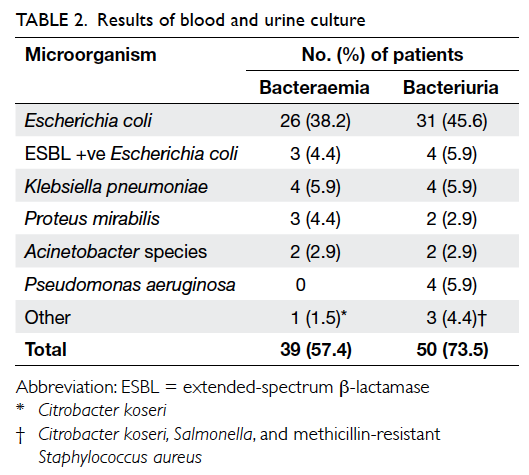
Microbiology
The yields of blood culture were positive in 57.4%
of the patients, with E coli being the commonest
causative organism (38.2%) followed by Klebsiella
pneumoniae, Proteus mirabilis, and Acinetobacter
species. Only three patients had bacteraemia caused
by extended-spectrum β-lactamase–producing E coli
(Table 2).
The prevalence of bacteriuria was 73.5%,
and E coli accounted for the majority of cases
with bacteriuria, followed by K pneumoniae and
Pseudomonas aeruginosa (Table 2).
Urological procedure
In addition to antibiotic administration, 75% (n=51)
of the patients required urological interventions,
including percutaneous nephrostomy (n=41),
insertion of ureteric stent (n=5), percutaneous
drainage (n=1), and nephrectomy (n=5).
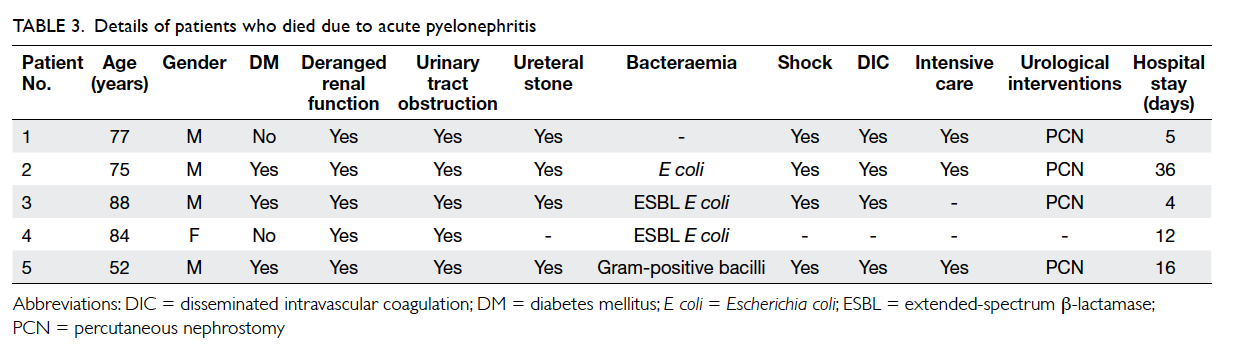
Mortality due to pyelonephritis
The overall mortality was 7.4% (n=5). Table 3
summarises the characteristics of patients who died
due to pyelonephritis within the same admission.
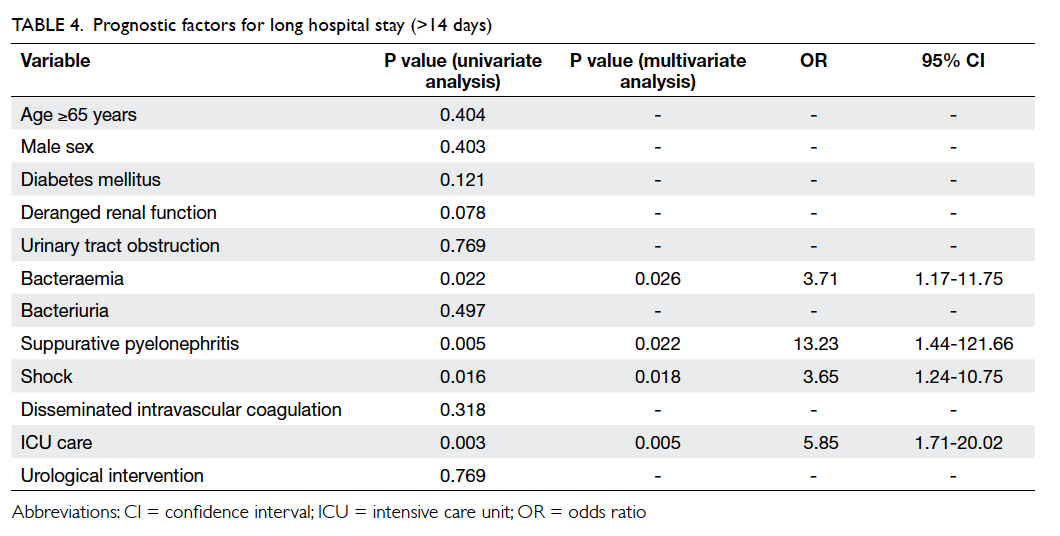
Prognostic factors for long hospital stay and
mortality
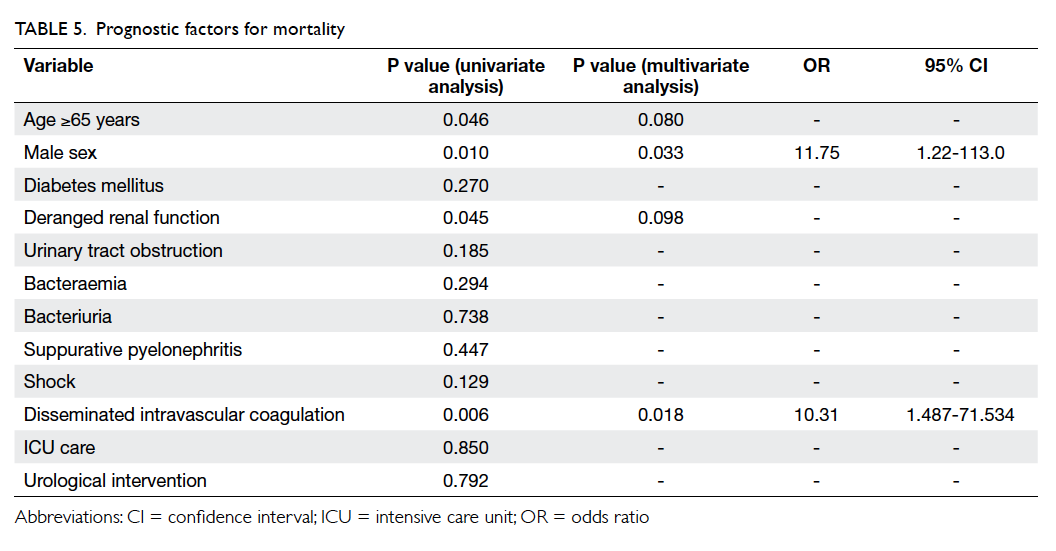
Risk factors for long hospital stay (>14 days; 32.4%)
and mortality (7.4%) were analysed (Tables 4 and 5).
Presence of bacteraemia (P=0.022), suppurative
pyelonephritis (P=0.005), shock (P=0.016), and need
for ICU care (P=0.003) were significant risk factors
for long hospital stay on univariate analysis. On
multivariate analysis, the odds ratios (ORs) were
3.71 for bacteraemia (P=0.026), 13.23 for suppurative pyelonephritis (P=0.022), 3.65 for shock (P=0.018),
and 5.85 for ICU care (P=0.005).
On univariate analysis, age of ≥65 years, male
sex, deranged renal function, and disseminated
intravascular coagulation (DIC) were predictors for
death. However, only male sex (OR=11.75; P=0.033)
and DIC (OR=10.31; P=0.018) were shown to be
independent risk factors in multivariate regression
analysis.
Discussion
Severe AP is an important disease entity that
frequently requires hospitalisation. Early recognition
of patients who are at risk of prolonged hospital stay
or even fatal events is important to improve treatment
results. Previous studies4 5 have shown a number of
risk factors including immunosuppression, old age,
and diabetes as risk factors for treatment failure. We
were interested in finding whether these risk factors
also applied to the local Hong Kong population.
An epidemiological study in the US found
that women are approximately 5 times more likely
than men to be hospitalised for AP; however, women
have a lower mortality rate than men.7 In our study
of hospitalised patients, females accounted for the
majority (70.6%) of AP cases. However, all but one
mortality from pyelonephritis occurred in the male
patients.
In one study on AP in adults, E coli was the
aetiological agent in 80% of the cases, but E coli
infections were less common in elderly patients
(60%). Furthermore, infections due to P mirabilis, K
pneumoniae, Serratia marcescens, and P aeruginosa
were very common due to the increased use of
catheters.2 Our study showed a similar microbial
spectrum. However, in AP, it is not always possible
to routinely document clinical UTI. This could be
attributed to previous antibiotic treatment, low
bacterial growth, or presence of atypical pathogens.8
In the present analysis, it was possible that a certain
proportion of patients had received antibiotic
treatment before admission to the hospital. Despite
this, the prevalence of bacteraemia and bacteriuria was relatively high (57.4% and 73.5%, respectively).
Escherichia coli accounted for the majority of
causative organisms.
An obstructed and infected kidney is a
urological emergency that may progress to septic
shock. Since acute obstructive uropathy raises the
renal pelvic pressure and, theoretically, decreases the
uptake of drugs by the kidney, emergency drainage
is warranted. A urological intervention significantly
increases the chances of good initial outcome.6 9
In this study, all patients who showed radiological
evidence of urinary tract obstruction were treated
with emergency drainage.
It has been suggested that bacteriuria and UTI occur more commonly in subjects with diabetes
than in the general population, and the risk of upper
tract involvement is also increased in these people.10
Diabetes seems to be associated with an increased
risk of severe UTI and unusual manifestations.11 12
The prevalence of diabetes in the present study was
also high (36.8%). In contrast with the results of
several studies, it was not shown to be a risk factor
for prolonged hospitalisation.4 5 The initial choice of
empirical antimicrobial therapy was not different
for diabetic patients, but we were more vigilant
for complications of UTI, such as emphysematous
pyelonephritis and abscess formation, in this group
of patients.
Recent reports4 13 have shown other risk
factors such as long-term catheterization and age of >65 years to be predictive of prolonged
hospitalisation. Our study revealed that four risk
factors—including bacteraemia, shock, need for
intensive care, and suppurative pyelonephritis—were associated with long hospital stay. These four
risk factors were closely related with and denoted the
most severe degree of pyelonephritis, thus resulting
in longer hospitalisation.
The mortality rate for patients with
pyelonephritis has been reported to be 1.2% to 33%.14 15
In our study, which included more severe group of
AP patients (ie those who required intensive care
or urological interventions), the overall mortality
rate was 7.4%. According to a previous study,4 septic
shock, bedridden status, age of >65 years, recent
use of antibiotics, and immunosuppression were
independent predictors of death. Another research
found that baseline health status of patients and
complexity of suppuration were the most important
predictors of clinical outcomes for suppurative
renal infections.6 In our analysis, patients who died
due to AP were predominantly older than 65 years,
presented with septic shock, and required drainage
for urinary tract obstruction. Among the risk factors
studied, age of ≥65 years, male sex, deranged renal
function, and DIC were associated with mortality
in univariate analysis. Additional multivariate
correlates were male sex and presence of DIC.
The limitation of the study was that the study
population consisted of a heterogeneous group
of patients and might not be representative of the
majority of uncomplicated AP cases. Presence of
resistant pathogens may contribute to treatment
failure, but we did not estimate this factor in our
analysis. Nevertheless, the outcomes of severe AP
also bear clinical implications for physicians who
mainly treat critically ill, hospitalised patients.
Conclusion
There was high prevalence of bacteraemia and septic
shock in patients with severe AP, with E coli being
the predominant causative organism. Male sex and presence of DIC were associated with mortality.
Early recognition of risk factors can potentially help
prevent death from severe AP.
References
1. Ramakrishanan K, Scheid DC. Diagnosis and management of acute pyelonephritis in adults. Am Fam Physician 2005;71:933-42.
2. Stamm WE, Hooton TM. Management of urinary tract infections in adults. N Engl J Med 1993;329:1328-34. CrossRef
3. Roberts FJ, Geere IW, Coldman A. A three-year study of positive blood cultures, with emphasis on prognosis. Rev infect Dis 1991;13:34-6. CrossRef
4. Efstathiou SP, Pefanis AV, Tsioulos DI, et al. Acute pyelonephritis in adults: prediction of mortality and failure of treatment. Arch Int Med 2003;163:1206-12. CrossRef
5. Pertel PE, Haverstock D. Risk factors for a poor outcome after therapy for acute pyelonephritis. BJU Int 2006;98:141-7. CrossRef
6. Stojadinović MM, Mićić SR, Milovanović DR, Janković SM. Risk factors for treatment failure in renal suppurative infections. Int Urol Nephrol 2009;41:319-25. CrossRef
7. Foxman B, Klemstine KL, Brown PD. Acute pyelonephritis in US hospitals in 1997: hospitalization and in-hospital mortality. Ann Epidemiol 2003;13:144-50. CrossRef
8. Rollino C, Beltrame G, Ferro M, Quattrocchio G, Sandrone M, Quarello F. Acute pyelonephritis in adults: a case series of 223 patients. Nephrol Dial Transplant 2012;27:3488-93. CrossRef
9. Yamamoto Y, Fujita K, Nakazawa S, et al. Clinical characteristics and risk factors for septic shock in patients receiving emergency drainage for acute pyelonephritis with upper urinary tract calculi. BMC Urology 2012;12:4. CrossRef
10. Stapleton A. Urinary tract infections in patients with diabetes. Am J Med 2008;113:80-4. CrossRef
11. Patterson JE, Andriole VT. Bacterial urinary tract infections in diabetes. Infect Dis Clin North Am 1995;9:25-51.
12. Lye WC, Chan RK, Lee EJ, Kumarasinghe G. Urinary tract infections in patients with diabetes mellitus. J Infect 1992;24:169-74. CrossRef
13. Roberts JA. Management of pyelonephritis and upper urinary tract infections. Urol Clin North Am 1999;26:753-63. CrossRef
14. Lee JH, Lee YM, Cho JH. Risk factors of septic shock in bacteremic acute pyelonephritis patients admitted to an ER. J Infect Chemother 2012;18:130-3. CrossRef
15. Yoshimura K, Utsunomiya N, Ichioka K, Ueda N, Matsui Y, Terai A. Emergency drainage from urosepsis associated with upper urinary tract calculi. J Urol 2005;173:458-62. CrossRef